Pain between Psyche and Soma in Uro-Andrology
Abstract
How to define pain? One of the most accredited definition is certainly “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage" (IASP (International Association for the Study of Pain - 1986) and World Health Organization (WHO) 1.
However, what are the essential components of pain experience? Certainly many factors are involved such as, among others:
Perceptual ability / suitability / subjective threshold;
The "subjective" experience;
Multidimensionality;
Occasionally or chronicity.
All these components have to be taken into consideration in the treatment of these disorders which, very often, require a multidisciplinary approach. From a clinical psychological point of view, much can also be offered at a diagnostic level, from the reception to listening to the patient's suffering, to the evaluation with standardized tests and psychophysiological analysis procedures in order to arrive at an effective personalization of treatments
Author Contributions
Academic Editor: Farah Yousef, Damascus University, Syria.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Carlo Pruneti, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
There is a whole series of psychological components, involved the chronic and recurrent pain that could be able to increase or decrease the pain perception. Among others, more or less serious incidence on personality characteristics, the problems posed by the vicissitudes of life and coping style a decrease in the quality of life, possible changes in the most intimate relationships, incapacity for work, an unwanted or undesirable change in interests.
Therefore, complexity characterizes any painful experience that has character of continuity / repetition with strong interconnection between body, or painful parts of it, and psyche. There are also different facets depending on the location of the pain and inevitable consequences for the subject-patient, the family and / or the cohabitants, the socio-cultural context with a global suffering, for the patient and for those who are close to him, those structures gradually. In a simple and perhaps a little coarse way, the pain can be considered corresponding to two major categories, acute and chronic (Figure 1).
There are also various characteristics related to the perception of pain for which we correctly talk about:
Discriminatory component, that is the ability of pain pathways to transmit spatial and temporal information on painful stimulus;
Cognitive component, that corresponds to the meanings attributed to the experience of pain;
Affective component since painful stimuli are always accompanied by emotional experiences.
There are also other psychological and psychopathological reaction common in all pain experiences: anxiety and depression (Figure 2).
Figure 2.Pain –Anxiety –Depression
Pain perception varies across different individuals according to their mood, emotional condition and prior experience, even if the pain is caused by similar physical stimuli and results in a similar degree of damage.
In 1965, Ronald Melzack and Patrick Wall 2 outlined a scientific theory about psychological influence on pain perception; the ‘gate control theory’.
If not for this theory, pain perception would be still associated with the intensity of the pain stimulus and the degree of damage caused to the affected tissue. But Melzack and Wall made it evident that pain perception is far more complex.
According to the gate control theory, pain signals are not free to reach the brain as soon as they are generated at the injured tissues or sites. They need to encounter certain ‘neurological gates’ at the spinal cord level and these gates determine whether the pain signals should reach the brain or not. In other words, pain is perceived when the gate gives way to the pain signals and it is less intense or not at all perceived when the gate closes for the signals to pass through. This theory gives the explanation for why someone finds relief by rubbing or massaging an injured or a painful area.
Though the gate control theory cannot present the complete picture of the central system that underlies pain, it has visualized the mechanism of pain perception in a new dimension and it has paved the way for various pain management strategies (Figure 3).
Figure 3.The Gate Control System, by Melzack and Wall 1965
Therefore, we can talk about pain as a total experience of the whole organism and, often, as already mentioned, with serious consequences in the subject's entourage who suffers a relapsing or chronic pain.
That obviously provoke strong repercussions primarily on a physical level but also at the psychological, social and working, interpersonal and relational levels and, why not, also spiritual (Figure 4).
Pain and Sexual Dysfunctions in Man
Sexual Dysfunctions are defined by DSM-5 as a heterogeneous group of disorders typically characterized by a clinically significant anomaly in a person's ability to have sexual relations or to experience sexual pleasure 3.
Sexual dysfunction are characterized by as a psycho-physiological modification within the various sexual phases such as interest, desire, excitement, orgasm and resolution. Another clinical condition is experiencing pain during sexual activity. Based on the origin of the disorder, organic sexual dysfunctions can be differentiated from psychogenic ones. We talk about organic etiology when it is believed that the cause is exclusively of physical nature or consequent to intake of particular drugs (e.g. antidepressants, anxiolytics, antipsychotics, antihypertensive, etc.) or substances (alcohol, cannabis, cocaine, heroin, etc.), we talk about psychogenic etiology when the genesis and the maintenance of the symptom are attributable exclusively to psychological factors. Furthermore, sexual disorder in men can be primary or secondary to another mental disorder.
In many individuals with sexual dysfunction, onset time can indicate different etiologies and types of intervention. The condition, in fact, can be permanent if it occurred from the first sexual experiences or acquired if it occurred after a period of relatively normal sexual performances. Again, situational sexual difficulties differ from generalized ones depending on whether the symptom is limited or not to certain types of stimulations, situations or partners.
Good sexual functioning, in fact, involves various aspects of individual's life. Therefore, during the assessment of sexual dysfunction, several aspects must be taken into consideration, relevant both for identifying the etiology and for choosing the most appropriate treatment; among these, there are factors concerning partner, relation, individual vulnerability, psychiatric comorbidity or stressful life events, culture or religion. It is ever important take into consideration the cultural factors that can influence expectations or generate prohibitions regarding the experience of sexual pleasure.
In fact, the sexual response is fundamentally biological, but intrapersonal, interpersonal and cultural context is generally experienced: therefore, it is believed that biological, psychological and socio-cultural factors interact between each other.
Education, unrealistic expectations, typical sexual interactions, beliefs and values, which can be the result of cultural learning and more or less positive experiences towards sex, can compromise the complete development of the sexual response.
Male sexual dysfunctions include delayed ejaculation, erectile disorder, male hypoactive sexual desire disorder, premature ejaculation, substance / drug-induced sexual dysfunction.
Another category that determines suffering on psychological level is that of painful syndromes that, both in acute and chronic manifestations, are prefigured as a stressful factor that the subject must constantly face.
The Psychological Component in Sexual Dysfunctions
All clinicians are aware that, even when dealing with sexual dysfunctions manifested on an exclusively organic basis, over time, a psychological mechanism can be linked the organic problem creating a loop which, over time, this may even worsen the clinical picture to the point of requiring psychiatric intervention.
In the case of erection deficit, for example, as in a self-fulfilling prophecy, fear, which becomes a negative expectation of failure from a sexual point of view, returns the failure itself as result. In most cases this happens because, during sexual activity, the attention is placed on, what are called, dysfunctional thoughts or negative anticipatory thoughts that are distracting thoughts as "I will make it!”, “Will I be able to achieve an erection?"," I have to get excited at any cost!".These thoughts create selective attention to dysfunctional stimuli, thus diverting attention from the functional ones, the sexually activating ones that are essential elements for a functional sexual response. This triggers a vicious circle in which sexual function is constantly undermined.
Many men with erectile disorder may have low self-esteem, low self-confidence and a reduced sense of masculinity and may experience depressive feelings.
Fear and / or avoidance of sexual intercourse can occur; this behavior can also interfere with the ability to develop stable and lasting intimate relationships. Usually this condition is associated with a decrease in sexual desire and satisfaction, an aspect that can cause interpersonal discomfort and cause disharmony within the couple, generating a vicious circle that feeds itself.
Erectile disorder can sometimes favor the onset of psychopathology or, in turn, be secondary to mental disorders such as anxiety and depressive disorders.
Certain anxiety disorders can also be associated with premature ejaculation.
Many males with this type of dysfunction, beyond the initial cause, complain of a sense of lack of ejaculation control and report feeling apprehensive about the expected inability to delay it in subsequent sexual intercourse. Therefore, over time, a control mechanism is triggered: the problem of wanting to control ejaculatory times arises and the solution adopted is to try not to "feel", to be distracted. But this increases the automatism because the basic problem is precisely the "not feeling" that leaves space for the imagination, much more immersive than the physical sensations.
In case of delayed orgasm, on the other hand, the opposite mechanism tends to be triggered: the man tries to accelerate the times by focusing on the concrete, on "feeling", leaving out the imagination, which is much more powerful and immediate.
Thus, sexuality becomes a very tiring and very boring practice.
Delayed ejaculation is often associated with significant psychological distress in one or both partners and can contribute to conception difficulties, for example; however, it is important to highlight that it can be a condition secondary to severe forms of major depressive disorder, which therefore take priority in treatment planning. In any case, it should be considered that various types of depressive reactions and other disorders characterized by low self-esteem, renunciation, social detachment, are often in comorbidity also with the male hypoactive sexual desire disorder.
Male sexual desire disorder is sometimes associated with concerns about erection and / or ejaculation: in fact, patients with this type of symptom often report that they no longer have sexual initiatives and that they are only minimally receptive to partner approaches.
As already mentioned above, even experiencing pain during sexual activity is a condition that can create psychological distress; moreover, this condition can occur in isolation or in comorbidity with other sexual dysfunctions. Although DSM-5 includes only genito-pelvic pain and penetration disorder, there are psychological manifestations of algic symptoms also in males.
The term “male dyspareunia” refers to the recurrent and persistent genital pain during erection, penetration, ejaculation or immediately after sexual intercourse. Often, even if not exclusively, the causes are urological; however, psychological repercussions must not be underestimated.
Sometimes, the avoidance mechanisms triggered by the fear of pain can promote the onset of the sexual aversion disorder where the avoidance of sexual genital contacts is total. In the clinical story of this kind of patients, it is not uncommon to find sexual violence and sexual relations experienced as traumatic and painful; these experiences are often accompanied by feelings such as guilt and shame.
However, subjective experiences are never univocal: we know, in fact, that stimuli endowed with the same stressful power do not necessarily provoke the same reaction in different individuals and stressful conditions of various entities can induce the same response in different people 4. The positive or negative interpretation is intimately connected to the inner physiological and psychological functioning involved in the interpretation of the world, so the high inter-individual variability is explained by the cognitive schemes, which are a sort of filter with which each person observes and understands reality 5. These mental constructions, in turn, are the result of various factors (stable personality traits, coping style, education, socio-cultural aspects) and therefore are flexible to adaptations made by new life experiences.
Temperamental factors, for example, play a fundamental role in the onset of sexual dysfunction. Neurotic personality traits, as well as submissive personality traits, can be associated with erection problems. Other predisposing factors for development and maintenance of sexual dysfunctions are alexithymia (the inability to process emotions at a cognitive level), which is positively associated with sexual dysfunctions with psychogenic etiology, but also anxiety disorders, and in particular social phobia in which fear is linked to the judgment of others.
Therefore, sexual dysfunctions can manifest themselves as mental disorders secondary to organic diseases or other mental disorders; however, it is also true that they favor the onset of other manifestations of psychological distress especially of anxious and / or depressive type.
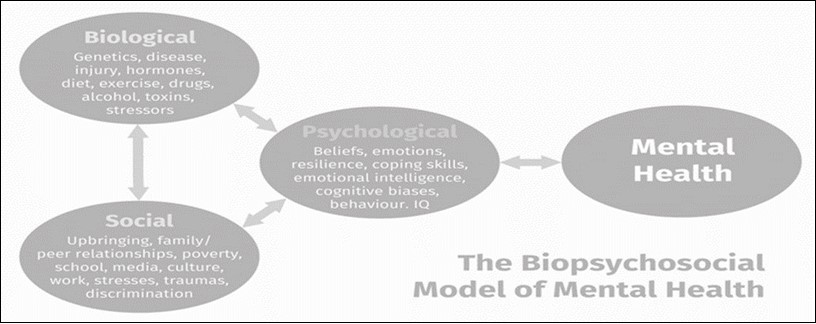
Following the biopsychosocial model of health 6, 7, 8 and considering the high coexistence of psychological distress in sexual dysfunctions, a correct diagnostic classification, involving the emotional-psychophysiological-social-cultural component but also the cognitive and behavioral one, is of fundamental importance (Figure 5).
Psychopathological Reactions, Anxiety and Depression
Anxious activation is part of everyday life: it is an index of adaptation of our body since it promotes the mobilization of useful resources to deal with certain stressful situations. However, if prolonged over time and without stressful stimuli, this activation can become not only useless but also harmful 4.
There are several studies that recommend screening for mental disorders frequently in comorbidity with chronic medical conditions, such as coronary heart disease 9, 10, 11 or diabetes mellitus 12, 13, 14, 15. In fact, only about half of patients with depression is identified in primary care practice 16, 17, 18. Self-administered screening tools can provide important information to healthcare professional in just few minutes 19.
A generic and useful tool for monitoring anxiety symptoms is the:
State Trait Anxiety Inventory(STAI-Y) 20, 21. The STAI-Y is divided into two scales (Y1 and Y2) which evaluate, respectively, state anxiety, referring how the subject feels at the time of the questionnaire administration, and trait anxiety with questions that investigate how the subject usually feels 22. In this way, it is possible to make a first discrimination between anxiety understood as symptom and anxiety expressed as habitual way of responding to external stimuli 23.
Beck Anxiety Inventory24 focuses more on the evaluation of hyperarousal (e.g. heartbeat, hand tremor, etc.) by investigating somatic and psychophysiological symptoms. BAI is particularly suitable for investigating the possible presence of panic, phobias or PTSD disorders 25.
Beck Depression Inventory26 is a self-report assessing the severity of depressive symptoms. It reliably assesses depression level and it is suitable for repeated administration 27.
Hamilton Rating Scale for Depression28 allows a reliable assessment of certain areas such as sleep disorders, libido and sexual functioning disorders, widespread somatic disorders, suicidal ideas, guilt and lack of energy.
Symptom Questionnaire29 is a self-assessment questionnaire that investigates the presence of any symptoms and the state of well-being/distress perceived by the subject in a specific period. It contains four scales based on the factorial analysis of psychological symptoms such as anxiety, depression, somatic symptoms and hostility. What makes this test particularly useful is the possibility to evaluate both the presence of specific symptoms and more cognitive aspects such as the ability or difficulty in relaxing, feeling pleasure, having a good disposition towards others. This test has a weekly, daily and hourly version, therefore particularly suitable for repeated administrations when the clinicians needs to monitor the progress of a treatment.
à P Stress Questionnaire30 is a self-report assessment tool, consisting of 32 multiple-response items concerning lifestyle and stress related habits, able to identify components at risk based on six rating scales identified with the factorial analysis.
The multidimensional approach to clinical diagnosis in psychopathology is usually made by collecting data from different aspects such as cognitive, behavioral, emotional and psychophysiological. For the purpose of a correct diagnostic classification, able to understand the various dimensions of the psychological distress, indexes like those proposed by DSM-5 cannot represent the only support in clinical diagnosis 31.
The psychophysiological evaluation (Psychophysiological Profile, PPP) 32 consists of detection, storage and evaluation of some of the physiological indexes connected with the Autonomic Nervous System (ANS) arousal and the complex system involved in stress response.
Recordings take place in three phases: baseline, stress (a stressor is administered, which can be objective - as in the case of the MAT in which the task is a serial subtraction - or subjective) and recovery (in which parameters are expected to return to baseline) 32, 33, 34. Sometimes a relaxation phase can also be entered.
The following are some of the most useful indexes for the evaluation of ANS: Peripheral Temperature (PT), Skin Conductance Response (SCR), Heart Rate (HR), Inter Bit Interval (IBI), muscle tension as indicated by the Surface Electromyogram (EMG) 31, 34.
Several studies have demonstrated the usefulness of this tool in making differential diagnosis in psychopathology 31, 34.
Both in diagnostic field and in treatment evaluation, there is Gray's Theory 35, integrated by the experimental contributions of Fowles 36, 37, which maintains that the increase in heart rate and in electro dermal activity is the physiological manifestation of, respectively, Behavioral Activation System (B.A.S.) and Behavioral Inhibition System (B.I.S.). The B.A.S., consisting in dopaminergic paths including the Ventral Tegmental Area (VTA) and the Nucleus Accumbens (NAcc), is activated by discriminative stimuli related to mostly positive reinforcements, but also to negative, if these ones are linked to pleasant events, and it rules the appetitive and fight or flight behavior. B.I.S. is, instead, a network of neural structures including Amygdala, Septo-Hippocampal System, receiving serotonergic afferents from Raphe Nucleus and noradrenergic afferents from Locus Coeruleus, and projecting an efferent to the Frontal Lobe. These structures, activated by discriminative stimuli mostly related to punishment or to the reinforcement interruption, are involved in the approach-avoidance conflict. In turn, these structures, leading to the consequent behavioral arrest and to the appearance of the defensive behavior of passive avoidance 4, 34.
In the field of clinical neurophysiology, several studies have shown the possibility of describing some psychopathological patterns by identifying physiological correlates. Thus, the anxious syndrome would be characterized by high levels of heart rate, muscle tone, electrodermal activity (level and response) and peripheral temperature decrease, while depressive syndrome would be distinguished by high levels of heart rate and muscle tone, but low levels of activity electrodermal (level and response) 4, 38, 39, 40.
Furthermore, in patients with obsessive-compulsive disorder, a pattern characterized by reduced autonomic activity configured by skin conductance, heart rate and electromyographic activity was observed 4, 41, 42, 43.
It is important to emphasize that the analysis of SCL / SCR can help in the differential diagnosis in clinical practice not only between anxious syndromes and depressive ones, but also between an episode of major depression and a picture of exhaustion in which the patient can be clinically depressed, but psychophysiologically still hyperactivated following a period of high stress.
A recent study conducted by Kim and colleagues 44 examined the stress response of patients diagnosed with Major Depressive Disorder using Electrodermal Activity (EDA) as the only parameter. In particular, the average amplitude of the Skin Conductance Level (MSCL), its standard deviation (SDSCL), the asymmetry of SCL (SKSCL) and the non-specific response of the skin conductance (NSSCR) in each of the five phases of the experimental protocol (baseline, stress, recovery, relaxation, recovery) were evaluated, as well as the differences between the phases in the same measured values. Another extremely relevant finding was the analysis of cardiac variability or heart rate variability or HRV. According to the authors, this modality is able to provide useful information by minimizing invasiveness, whether or not to corroborate the diagnostic classification data based on the observation and description of symptoms such as DSM 45.
These authors 44 have also shown that the analysis of these parameters is able to detect the presence of Major Depressive Disorder (MDD) with an accuracy of 74%, by means a decision tree algorithm MDD vs control groups selected on the basis of five parameters (apolipoprotein B, specific component of the group, ceruloplasmin, RMSSD and SampEn) with an accuracy of 80.1%.
In this study 44 it was concluded that a combination of HRV, SCL analysis and proteomic data achieved exceptional precision in the classification of the disorder and its sizing with a contribution of almost 45% only to the HRV, confirming in part also previous and contemporary studies 46, 47.
In addition, these authors also highlighted that the ability to discriminate increases if one takes into account the difference between the levels of physiological parameters detected in the stress phase and in the relaxation phase. This is the most useful aspect for both diagnostic and therapeutic purposes as it is important to detect the psychophysiological stress reaction but it is equally important to describe emotional self-regulation ability, which allows the recovery of psychophysical balance.
The Psychophysiological Profile can also be useful assessing any algic symptoms by measuring the levels of physiological parameters following the administration of a stressor that can also be imaginative.
Further and recent studies have investigated autonomic reactions more widely following the presentation of stimuli with emotional content 48, 49, 50. In a study conducted by Lelard and collaborators in 2017 48, an increase in heart rate (HR) values was found in the conditions in which the participants underwent a mental imagination task concerning a painful sensation experienced in first person.
What is described on experimental level can also be very useful in clinical setting: subjecting a patient who complains of a form of pain to basic and stress Psychophysiological Profile, allows obtaining a lot of information about his level of pain endurance, but also about the intensity of algic symptomatology. Observing its autonomic response in the three recording phases: baseline, stress administration and recovery.
It may be useful to integrate this investigation with the administration of a simple test to assess the intensity of pain experienced (semantic differential, visual analogue etc.).
Quantitative” characteristics of pain are assessed through semantic, numerical or linear scales. Among others, the Semantic Differential 51 can be useful and that allows investigating the meaning that certain concepts of life have for the subject by highlighting three dimensions that are evaluation (eg. Good-Bad), power (e.g. Strong-Weak) and activity (eg. Active-Passive).
Instead, numerical scales require the patient to indicate the intensity of pain with a numerical value indicating with 0 the absence of pain and with 10 an extreme pain, considering the central values as representative of the shades in between.
Finally, the analogue-visual scales allows visualizing pain by dividing a segment with a line that represents its intensity from absent to extreme.
Integrating the various information obtained from the different diagnostic tools, allows investigating the patient's psychophysical balance and its methods of processing information: both explicit (cognitive) and tacit (emotional) ones.
Thus, a psychophysiological profile characterized by high reactivity to the stressful stimulus (imagination of one's pain), but denied explicitly, allows to detect the poor ability to mentalize one's pain and, indeed, the tendency to neglect/deny proprioceptive - nociceptive stimuli and the emotional consequences of it.
A profile characterized by low reactivity to stress, in a person who declares high levels of pain, can be indicative of a low or very low pain threshold.
Furthermore, a patient who declares high levels of pain and whose psychophysiological profile is characterized by hyperarousal could experience the pain at more intense level than another with normal or balanced sympatho-vagal response. In addition, in this case, however, both the response to stress and the ability to recover is fundamental: the approach to be adopted with a subject who is able to return to baseline conditions will be different from a subject who instead struggles to recover basal values.
The perception of pain, then, understood as the perceptual component (nociception) linked to the transmission of the painful stimulus to the brain, is a very complex process in which the psychological dimensions play a preponderant role. From the very concept of perception, or "recognition of sensation”, with the various concepts connected to it, such as the perceptual threshold partially influenced by the contents learned which are capable of influencing each individual.
According to the studies of Porges and colleagues 52, 53, growth in interpersonal relationships could activate the ventro-vagal complex, the so-called Social Engagement System, SES. These subjects are characterized by the perception of better interpersonal relationships, as well as the actual emotional expression could activate this system, which, through the myelin branch of the vagus nerve, activates visceral states of relaxation and calm; and the opposite is true. Visceral states of relaxation and calm could facilitate the activation of Social Engagement System and, consequently, a possible growth in relations with others.
If this were confirmed by further research, it could be argued that post-traumatic growth also has a physiological effect: in fact, it could stimulate the vagus nerve which, hindering the activation of the Sympathetic Nervous System, could inhibit oxidation, inflammation and metastasis processes. This chain of physiological events could thus guarantee a better prognosis for these patients.
Finally, significant correlations emerged between the quality of life and the body image.
A defective emotional functioning is associated with a negative self-perception. The negative self-concept could compromise the emotional functioning of many andrological patients. Basis on what emerged from the literature, it is hypothesized that the distress resulting from a negative perception of one's own body image or pain resulting in hypofunctionality, usually has an impact on emotional functioning, in terms of anxiety, tension, concern, irritability or even depressive states. On the contrary, a positive self-perception could guarantee and support a good emotional functioning. There could even be a second hypothesis, based on an opposite direction to the previous one: the distress, in fact, could be caused by already previous poor emotional functioning of these patients, which could lead to rigidity about the perception and the attention in the body, and ultimately to a negative self-perception disproportionate to the circumstances.
Finally, physical pain is significantly related to lower awareness of his own face, appearance in general and more positive self-perception. In andrological patients, it seems that high pain symptomatology contributes to more negative self-perception in general and to less concerns about their general appearance including face. These reactions would seem paradoxical, because physical pain would facilitate to focus the negative attention on their own body and on themselves.
In any case, all these data lean towards a non-superficial and always multidimensional and multidisciplinary clinical evaluation in order not to incur in diagnostic errors and only apparently adequate therapies. Remember, just to give an example, that a medical prescription always needs an adequate "compliance" or adherence to dosage and duration to be effective. People with a previous inadequate psychic and emotional balance, or frustrated by chronic and relapsing pain, perhaps even resistant to previous treatments, it is very likely that will run the risk of poor compliance mainly due to depressive symptoms or characteristics.
In light of this, it is not surprising that recent experimental studies have even shown an increased pain perception threshold in depressed subjects compared to healthy controls. It has been hypothesized that the interceptive sensitivity is altered following a decreased serotonergic and noradrenergic transmission at the level of the descending (inhibitory) control pathways of the synapses, that control the transmission of chronic pain and / or of visceral origin (at the level of the Periaqueductal Gray) and / or abnormal activation of pro-inflammatory cytokines and substance P 54, 55, 56, 57, 58.
For further study of these concepts, please refer to the numerous texts on this subject, but a summary is a must: “biologically and phylogenetically the human race is predisposed to have the best levels of social, emotional, sexual interaction, or, in any case, based on love, affection and consideration, in a state of alert relaxation and rest, not of excitement”.
A proof is found, for example, at the level of the male sexual response: the tumescence and erection of the penis are managed precisely by the Parasympathetic Nervous System, a system usually inhibiting, while ejaculation and orgasm, is managed by the Sympathetic Nervous System (usually an activator). A physiological and functional proof that, in situations of chronic stress and need of a particular activation of the organism certain physiological function could be altered.
In the described situation, if the organism (like a mind-body integration system) not realize that there are the ideal conditions of relaxation, calm and tranquility for the Parasympathetic-Vagal stimulation of penile tumescence, if it does not "feel safe", free of negative thinking and feelings, that does not will allow an adequate erection.
The relationship between depression and painful symptoms is complex, widely studied in the literature, and probably recognizes a bidirectional causality that provides different explanatory models.
One of the most explanatory models studied, especially in the clinical setting, has been that of depression as a psychological reaction consequent to the chronicity of the painful condition: pain would facilitate the development of a depressive condition resulting from the functional limitations related to painful symptoms.
In the opposite case, it can be hypothesized that the depressive clinical condition may influence the nociceptive transmission by altering the threshold of perception of pain or by causing a chronic inflammatory phenomenon that favors its onset 54, 55, 56.
Psychological Intervention and Treatment
Psychotherapy should always be carried out by dedicated psychotherapists licensed clinical psychologist (PhD and PsyD) or physicians (MD psychiatrist) and with masters and advanced courses in sexology, and both the referral and the discussion about the patient must always be shared with the specialist doctor. Therapy often have to be integrate, psychological and pharmacological. The last one, prescribed by the reference urologist/andrologist, even if teamwork is always wise to define the treatment of excellence, agreed between specialists, for those painful syndromes associated with sexual disorders with an important psychological component 60, 61, 62.
Cognitive-behavioral therapy has shown the highest scientific evidence of effectiveness in this area. It is a type of strategic intervention, aimed for the symptom, short (10-15 sessions); it can be individual or as a couple, but, since sexual dysfunctions manifest their disturbance in the context of the relationship with the partner, it is in couple psychotherapy that maximum results are obtained, also going to act on the relationship.
The psychotherapist tries to solve the vicious circle that feeds the problem and that leads the person to increase the levels of emotional activation (tension, anxiety, fear, anger, shame, sadness, etc.) losing, in most cases, pleasure in sexual activities and leaving room for the concern that these symptoms cause. Focus the attention on the problem, the symptom, the pain or the performance, leads the body to an involuntary attempt to reduce the tension states that develop the symptom, many times inhibiting sexual desire.
The therapist uses cognitive and behavioral techniques, capable of reorganizing the natural processes of the organism in a functional sense. Therefore, the active role of the individual (or the couple) is required, who will be asked, from time to time, to carry out erotic-educational exercises in their intimacy, which, according to a detailed protocol, will be assigned during the therapeutic course. The goal is to create a climate of cooperation in a context in which performance is not important and to eliminate the dysfunctional emotions associated with sexuality, thus restoring a dimension of pleasure.
As a patient suffering from a painful form of Peyronie’s Disease said: “When that part of my body causes me pain, I feel that the ability to be with myself, with others, with the rest of the world is also compromised”.
Hence the importance of dealing with it and treating it from a psychological point of view.
Pain, in fact, is not just a response to a physical stimulus recorded by the central nervous system, which causes an unpleasant sensation. The nociceptive stimulus is transmitted in the spinal cord and in the brain but the signal does not reach a single and specific pain center; on the contrary, the information spreads to various brain areas responsible for interpretation, evaluation and emotions.
In addition, past pain experiences, fears attributed to it, perception of being able to cope with it, medical, relational and social support and many other factors determine the way in which pain is experienced and our reaction to it.
Illness and pain experience in the body can often be connected to a psychic situation of "impasse", of relational constraint ("neither with you, nor without you"), of imposed identity ("I can't be what I am, but I must be what others expect from me”).
The specialists of the UPMC Brain Clinic Salvator Mundi International Hospital consider that the prerequisites of contemporary relational psychosomatic medicine are essential: the state of health (physical and mental) is linked to pleasure feelings, that derives from the use of one's own body, one's own thought and one's own imagination.
Associated with the concept of pain, there is the concept of disability (understood as the loss of previously acquired functioning skills). In these cases, physical disability must be associated with the recognition of "emotional disabilities": numerous studies report that chronic pain is associated with depressed mood, anxiety, post-traumatic stress disorder, typical avoidance behaviors, fixity and emotional stasis. It also emerges from research that patients suffering from chronic pain show a decrease in the ability to remember dreams (indicating a decrease in the duration and frequency of REM sleep), or the tendency to remember only "traumatic dreams", in the form of nightmare, which in turn report the traumatic experience of disease and disability.
The psychotherapist can help the patient to know and feel not only the pain, but also expand the possibility to feel all the sensations. In this way will be possible to appreciate the obtained achievements, such as, for example, the results of a physical rehabilitation program in a patient with fibromyalgia or the results of the positive outcomes of a surgical intervention, so that the experience of evolving and gaining mastery over oneself can be “metalized".
Among others, specialists of the UPMC Salvator Mundi International Hospital Brain Clinic in Rome take care of the "subjective body", that is, what can be defined as a "painful identity" of a given individual, at that time. Therefore, psychotherapy cannot only be aimed at the best possible pain management, but also at a deep understanding of it, in order to provide adequate, even analgesic of course, care but which cannot, and must not, be separated from the whole person. The attempt that the psychotherapist must carry out is to support the patient go from "it hurts" to "I feel bad because that part of me is painful". So the vision changes and the request that is also made to the doctor becomes different, with an adequate accent on the suffering that accompanies pain in almost all its manifestations.
It is therefore necessary to adopt a multidimensional and multidisciplinary approach that plans an integrated and individualized care intervention, paying attention to the person as a whole. This kind of approach pays attention to the narration that the patient makes, starting from an accurate description of medical history, with particular emphasis on the events remembered as important, stressful, and stimulating the individual in the accurate description of this life-events end the type of feeling during the remembering 63.
Of course, medical and psychological team will have to discuss together the type of intervention according to the clinical situation. In andrology, for example, psychological, emotional and relational concomitances will be of great importance. It may be important, for example, to discuss the need for immediate intervention that, almost magically, can take away the pain, but may not help the person to identify what is really missing in his life.
I recall here a recent clinical case of a patient, sent by the treating physician, who felt penis pain with a syndrome that remembered, but was not exactly coincident with, Peyronie’s Disease. Only after several diagnostic interviews, a picture similar to that described by Alfred Hitchcock's film "Psycho" emerged. The patient, in fact, was full of anger towards the maternal figure, with which he had always lived and with whom he completely confided. He never had a girlfriend and a sexual relationship and had used, maybe even abusing on it, artificial vaginas until provoking a real ulceration on one side of the penis. This also after having also undergone a surgical operation by a urologist to try to "straighten" the slightly curved penis near the base. During the first visits in my study, was also examined by a dermatologist who was able to mitigate the pain with a cortisone treatment. After this, he never showed up again to the treatments that probably, at that point, would have to be both psychiatric and psychotherapeutic.
In recent years, within the vast panorama of clinical psychology and its applications, the need to approach pain has emerged more and more, in particular chronic pain and its various components in order to better offer support primarily to patients.
That can be done with a real multidisciplinary approach and, therefore, to psychologists and psychiatrists colleagues, in order to be able to better manage the sufferings of patients, but also to the other health professionals, who may be interested in knowing psychological aspects of pain to improve their care activities.
In fact, it is not possible to cure and, above all, take care of people with pain without a solid and continuous medical and clinical-psychological training.
When dealing with human beings, certainties and dogmas must be reduced in order to observe, listen and learn the multifaceted and ever new language of the body.
The effectiveness of a warm and loving welcome, of attentive and unhurried listening, of non-hasty reassurances and the offer of emotional availability over time are necessary values for a complete approach to the person who may already be able to mitigate, even if probably not solve, anxieties, fears and anguish of illness and death with consequent abandonment, loneliness, depression. An adequate and personalized acceptance can also amplify the power of the drug, which, if properly prescribed, even if not strictly necessary, can be extremely useful for the best management of pain syndromes such as those affecting the male genitalia.
References
- 3. (2013) American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author .
- 4.Pruneti C. (2019) funzionale in psicologia clinica e psicopatologia. Bologna: Società Editrice Esculapio.
- 5.Pruneti C. (2016) Positive Psychology: Old and New Theoretical Requirement for “Living this. , Moment”.J Depress Anxiety 5, 242.
- 6.G L Engel. (1977) The need for a new medical model: a challenge for biomedicine.Science. 196(4286), 129-36.
- 7.G L Engel. (1980) The clinical application of the biopsychosocial model.American. , Journal of Psychiatry 137(5), 535-544.
- 9.C Jordan Albus, Herrmann-Lingen J, C. (2004) Screening for psychosocial risk factors in patients with coronary heart disease-recommendations for clinical practice. Eur J CardiovascPrevRehabil,11:. 75-79.
- 10.Janeway D. (2009) An integrated approach to the diagnosis and treatment of anxiety within the practice of cardiology.Cardiol. , Rev 17, 36-43.
- 11.Schussler G, Heuft G. (2008) Anxiety and depression in patients with medical diseases. , Z Psychosom Med Psychother 54, 354-367.
- 12.Bernstein C M Stockwell, M S Gallagher, M P Rosenthal, S L, K. (2013) Mental health issues in adolescents and young adults with type 1 diabetes: prevalence and impact on glycemic control. Clin Pediatr(Phila). 52, 10-15.
- 13.Hall P A Coons, M J Vallis, M T. (2008) Anxious temperament and disease progression at diagnosis: the case of type 2 diabetes. , Psychosom Med 70, 837-843.
- 14.M Hendrikz, Dann J, Kenardy F, J. (2008) Screening for depression in patients with diabetes mellitus. PsychosomMed. 70, 869-874.
- 15.Pouwer F. (2009) Should we screen for emotional distress in type 2 diabetes mellitus? NatRev Endocrinol,5:. 665-671.
- 16.J Volkers Nuyen, A C Verhaak, P F Schellevis, F G Groenewegen, Bos P P Van den et al. (2005) Accuracy of diagnosing depression in primary care: the impact of chronic somatic and psychiatric comorbidity. Psychol. , Med 35, 1185-1195.
- 17.M D Seelig, Katon W. (2008) Gaps in depression care: why primary care physicians should hone their depression screening, diagnosis, and management skills. J Occup Environ. , Med 50, 451-458.
- 18.Sherbourne C D Wells, K B Hays, R D, Burnam W, M A Judd et al. (1994) Subthreshold depression and depressive disorder: clinical characteristics of general medical and mental health specialty outpatients. Am J Psychiatry,151:. 1777-1784.
- 19. (2014) US Preventive Task Force (USPSTF,2014). Screening for Depression. Recommendations and Rationale.
- 20.Spielberger C D Gorsuch, R L Lushene, E R. (1970) for the State-Trait Anxiety Inventory (Self Evaluation Questionnaire). Palo Alto. , CA:ConsultingPsychologistsPress
- 21.RL Lushene Gorsuch, Vagg R, Jacobs P R, GA. (1983) Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting sychologists Press.
- 22.E Sanavio Franceschina, Sica E, C. (2004) I disturbi d’ansia. In: Galeazzi, A.& Meazzini, P. (Acuradi) Mente e comportamento. Trattato italiano di psicoterapia cognitivo-comportamentale, Milano: Giunti Editore.
- 23.Lingiardi V. (1991) L’ansia: riferimenti semeiologici. In: Smeraldi, E. Bellodi, L. Provenza, M. A. proposito dell’ansia. In: Smeraldi,E.&BellodiL.(Acuradi). I disturbi d’ansia.Clinica e terapia, Milano:edi-ermes.
- 24.Beck A T Epstein, Brown N, Steer G, A R. (1988) An inventory for measuring clinical anxiety: Psychometric properties. , Journal of Consulting and Clinical Psychology 56(6), 893-897.
- 25.Rose M, Devine J. (2014) Assessment of patient-reported symptoms of anxiety.Dialogues in. , Clinical Neuroscience,16 2, 197-211.
- 27.L E Beutler, Crago M. (1983) Self report measure of psychotherapy outcome. In: Lambert, M. Christensen, E. DejulioS. The assessment of psychotherapy outcome. , New York: WileyandSons
- 28.Hamilton M. (1967) Development of a rating scale for primary depressive illness. Hopkin University Press.
- 29.Kellner R. (1976) Abridged manual of the Symptom Questionnaire. Albuquerque:University of. , New Mexico
- 30.Pruneti C. (2011) The « P Stress Questionnaire »: A new tool for the evaluation of stress-related behaviours, Europ.J. of Clinical Psychology and Psychiatry, VI 3, 1-37.
- 31.C Saccò Pruneti, Cosentino M, Sgromo C, D. (2016) . Relevance of Autonomic Arousal in the Stress Response in Psychopathology.Journal of Basic & Applied Sciences 12, 176-184.
- 32.Fuller D. (1979) Biofeedback methods and procedures in clinical Practice. S.Francisco: Biofeedback Press.
- 33.T Braune Hoehn, Scheibe S, Albus G, M. (1997) Physiological, biochemical and subjective parameters in anxiety patients with panic disorder during stress exposure as compared with healthy controls.European Archives of Psychiatry and Clinical Neuroscience. 247(5), 264-274.
- 34.Pruneti C, Cosentino C, Sgromo M, Innocenti A. (2014) Skin Conductance Response as a decisive variable in individuals with a DSM-IV TR Axis I diagnosis. JMED Res.565009.
- 36.D C Fowles. (1980) The three-arousal model: Implications of Gray’s two-factor learning theory for heart rate, electrodermal activity, and psychopathy. Psychophysiology. 17, 87-104.
- 37.D C Fowles. (1988) Psychophysiology and psychopathology: A motivational approach.Psychophysiology. 25, 373-391.
- 39.M H Lader. (1975) The psychophysiology of anxious and depressed patients. , In Fowles, D. C. (acuradi),Clinical applications of psychophysiology. NewYork: Columbia University Press
- 40.M H Lader. (1983) Anxiety and depression. In Gale,A.&Edwards,J.A.(eds.). Physiological correlates of human behavior. Londra: Academic Press .
- 41.Lelliott P T, Noshirvani H F, Marks I M, Monteiro W O, Basoglu M et al. (1987) Relationship of skin conductance activity to clinical features in obsessive-compulsive ritualizers. , Psychological Medicine 17(4), 905-14.
- 42.S McLeod Hohen, D R Hipsley, P. (1995) Is hyperarousal essential to obsessive-compulsive disorder? Diminished physiologic flexibility, but not hyperarousal, characterizes patients with obsessive-compulsive disorder.Archives of General Psychiatry. 52(8), 688-93.
- 43.Zahn T P Leonard, H L Swedo, S E Rapaport, L J. (1996) Autonomic activity in children and adolescents with obsessive-compulsive disorder.Psychiatry. , Research 60, 67-76.
- 44.Kim A Y Jang, E H Kim, Choi S, K W Jeon, H J Yu et al. (2018) Automatic detection of major depressive disorder using electrodermal activity. , Sci Rep 8, 17030.
- 45.Poh M Z Swenson, N C Picard, W R. (2010) A wearable sensor for unobtrusive, long-term assessment of electrodermal activity.IEEE. , Trans. Biomed. Eng.57 1243-1252.
- 46.J M Gorman, R P Sloan. (2000) Heart rate variability in depressive and anxiety disorders.Am Heart. , J 14(4), 77-83.
- 47.R Schmidt Hartmann, F M Sander, Hegerl C, U. (2019) . Heart Rate Variability as Indicator of Clinical State in Depression 9, 735.
- 48.T Godefroy Lelard, Ahmaidi O, Krystkowiak S, Mouras P, H. (2017) . Mental Simulation of Painful Situations Has an Impact on Posture and Psychophysiological Parameters. Front. Psychol.8: .
- 49.T Krystkowiak Lelard, Montalan P, Longin B, Bucchioni E, G. (2014) Influence of postural threat on postural responses to aversive visual stimuli.Behav. Brain Res.266. 137-145.
- 50.Lang P J Bradley, M, B N Cuthbert. University of Florida (2008) Affective Picture System (IAPS): Affective Ratings of Pictures and Instruction Manual.Gainesville, FL:. Technical Report A-8
- 51.Osgood C E. (1957) Method and theory of experimental psychology. , New York: OxfordUniversityPress
- 52.Porges S W. (2011) The Polyvagal Theory: Neurophysiological Foundations of Emotions. , Attachment, Communication, and Self-regulation. W .W. Norton & Company
- 53.Corrigan Frank E M. (2014) Neurobiology and treatment of traumatic dissociation toward an embodied self. , NewYork: Springer 510.
- 55.J Clauw Goesling, D J Hassett, L A. (2013) Pain and depression: an integrative review of neurobiological and psychological factors. CurrPsychiatry Rep. 15(12), 421.
- 56.J Gattner, Jaracz K, Górna K, K. (2016) . Unexplained Painful Physical Symptoms in Patients with Major Depressive Disorder: Prevalence, Pathophysiology and Management.CNS Drugs 30(4), 293-304.
- 57.T Correll, C U Gallop, Vancampfort K, Stubbs D, B. (2016) Is Pain Perception Altered in People With Depression? A Systematic Review and. , Meta-Analysis of Experimental Pain Research.J Pain 17(12), 1257-1272.
- 58.C Blom Benatti, J M Rigillo, Alboni G, Zizzi S, F. (2016) . , Disease-Induced Neuro inflammation and Depression.CNS Neurol Disord Drug Targets, 15 4, 414-33.
- 59.Rijavec N, V N Grubic. (2012) Depression and pain: often together but still a clinical challenge: a review.Psychiatr Danub. 24(4), 346-52.
- 60.Payne K A Binik, Y M Amsel, Khalifè R, S. (2005) When sex hurts, anxiety and fear orient attention towards pain. Eur. , J Pain; 9(4), 427-36.
- 61.S Everaerd Both, Laan W, E. (2007) Desire emerges from excitement: a psychophysiological perspective on sexual motivation. In: Janssen E, editor.The psychophysiology of sex. , Bloomington (IN):IndianaUniversityPress, 327-39.
Cited by (2)
This article has been cited by 2 scholarly works according to:
Citing Articles:
International journal of psychological research (2023) OpenAlex
S. Guidotti, C. Pruneti, Simona Mortilla, G. Masellis, Chiara Caramuscio - International Journal of Psychological Research (2023) Semantic Scholar