Determinants of Exclusive Breastfeeding Among Mothers of Infants Less Than Six Months of Age in Mogadishu: A Facility-Based Cross-Sectional Study
Abstract
Background
Breastfeeding is a vital practice for infant health and well-being, with exclusive breastfeeding (EBF) during the first six months being particularly crucial. Despite its benefits, EBF is sub-optimally practiced in many low-to-middle income countries. This study focuses on Somalia, a country with historical political instability and poor health indicators, aiming to identify the prevalence and determinants of exclusive breastfeeding among women with infants under six months attending SOS Mother and Child Hospital in Mogadishu.
Methods
A hospital-based cross-sectional design was used, and data were collected through a structured questionnaire. The study sample consisted of 345 mothers, selected using a systematic sampling technique. Descriptive, bivariate, and multivariate analyses were conducted to assess breastfeeding practices and determine factors influencing exclusive breastfeeding prevalence.
Result
The study found that the prevalence of exclusive breastfeeding among the study population in Somalia was 44%, influenced by factors such as maternal education, employment, and utilization of antenatal and postnatal care services. Male infants and younger infants had higher odds of being exclusively breastfed.
Conclusion and recommendations
The study emphasizes the importance of promoting exclusive breastfeeding as the optimal feeding practice for infants in Somalia, highlighting the need for comprehensive health education during antenatal care visits and postnatal counseling. It recommends the development of supportive policies, such as maternity leave and workplace accommodations, along with community-based initiatives and support groups to facilitate and encourage exclusive breastfeeding practices.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2024 Hassan Abdullahi Dahie, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Background
Breastfeeding is a vital practice that contributes significantly to the health and well-being of infants1. Exclusive breastfeeding, defined as the provision of breast milk alone to infants during the first six months of life without the introduction of any other liquids or solids, is particularly important for optimal growth, development, and disease prevention. Breastfeeding is critical for sustaining the health and well-being of newborns and infants2. Breast milk is a unique source of food for babies which contains all necessary nutrients that will ensures the infant's health, growth and development3. This source of food cannot be replaced with any other diet, as breast milk contains numerous antioxidants, protecting babies against harm caused by pathogens4, 5. Increasing evidence suggests that initiating breastfeeding early, ideally within the first hour after birth, has a noteworthy effect in decreasing neonatal mortality rates6. Infants who are properly breastfed grow better and experience less sickness and fewer deaths than infants who are not breastfed7. Encouraging exclusive breastfeeding is the most efficient and economically viable strategy to decrease infant mortality in developing nations.
Additionally, breast milk contains antibodies passed on from the mother, which aid in fighting diseases and protecting infants from conditions such as diarrhea and acute respiratory infections8. Moreover, breastfeeding stimulates the immune system of the baby and enhances their response to vaccinations. Some studies suggest that breastfeeding may also have cognitive benefits7, 8, 9, 10. Furthermore, if breastfeeding continues beyond six months alongside the introduction of nutritionally adequate, safe, and appropriate solid, semi-solid, and soft foods, it contributes to maintaining good nutritional status and offers protection against illnesses.
Despite the known benefits of exclusive breastfeeding (EBF) and various efforts to promote its practice, the reality remains that EBF is sub-optimally practiced in many low-to-middle income countries9. This may be influenced by factors such as limited knowledge and awareness, cultural beliefs, lack of support and education, maternal employment constraints, aggressive marketing of breast milk substitutes, and a lack of breastfeeding-friendly environments10.
The study aims to address the unique circumstances of Somalia, a country with a history of political instability and poor health indicators, by specifically focusing on identifying the prevalence and determinants of exclusive breastfeeding among women with infants less than six months old attending at SOS Mother and child hospital, Mogadishu.
Methods
Study setting and design
A hospital-based cross-sectional design was adopted using a quantitative approach. The study was conducted within SOS Mother and Child Hospital, which serves as a tertiary healthcare facility specializing in maternal and child healthcare. With a bed capacity of around 150 beds, the hospital caters to beneficiaries from various regions across the country.
Population
In this study, the target population consisted of mothers who have infants aged less than six months and who sought healthcare services at SOS Mother and Child Hospital in Mogadishu.
Sample size
The sample size of this study was calculated using single proportion formula of sample size determination with the following assumptions: previous proportion of 34% of exclusive breastfeeding based on government data11, 95% confidence and margin of error of 5%. Using the Kish and Leslie formula12 for sample size determination, a sample size of 345 mothers was obtained. To cater for the non-response rate, a sample size of 384 was finally taken.
n=(1.96)2.0.34(1-0.34)/(0.05)2
Therefore, 345 participants were interviewed.
Sampling technique
The study employed a systematic sampling technique to select participants from the target population. The sampling frame was constructed using the hospital's registration records, which contain information on mothers and their infants who seek healthcare services at the hospital. The sampling frame included all eligible mothers within the specified age range attending the hospital during the study period. The sampling interval was calculated by dividing the average total number of eligible mothers attending the hospital during the study period by the desired sample size. The first participant was selected randomly using this random number. Subsequently, every nth participant has been selected until the desired sample size is reached.
Data collection procedure and data quality control
Participants were recruited from the target population, which includes mothers with infants aged less than six months attending SOS Mother and Child Hospital in Mogadishu, Somalia. Eligible participants who were identified from the hospital's registration records through systematic random and approached by trained research personnel. The questionnaire underwent a pilot test to assess its clarity and understandability. Any feedback received during the pilot test was taken into consideration to make the necessary adjustment to the questionnaire.
Study instrument
The study used a structured questionnaire to collect data. The questionnaire was developed based on relevant literature and previous studies on breastfeeding practices. It included questions on demographic characteristics, breastfeeding practices, knowledge about exclusive breastfeeding, and factors influencing breastfeeding decisions.
Measurement of variables
Dependent Variable
The dependent variable in this study is the prevalence of exclusive breastfeeding. These variable measures the proportion of mothers who exclusively breastfeed their infants, meaning that they provide only breast milk without any other liquids or solids except for vitamins, minerals, or medication. It was determined through interviews or questionnaires with the participating mothers.
Independent Variables
The independent variables were factors that may influence the exclusive breastfeeding practices. These variables include maternal age, education level, household socioeconomic status, maternal occupation, parity (number of previous children), maternal knowledge about exclusive breastfeeding, maternal attitudes towards exclusive breastfeeding, social support received by the mother, infant age, and infant sex. These variables were collected through interviews or questionnaires to assess their association with exclusive breastfeeding prevalence.
Data analysis
The collected data were checked for accuracy, completeness, and consistency. Any missing or erroneous data points was addressed through data cleaning procedures. Following the proper preparation and organization of dataset for analysis, descriptive analysis was performed to summarize the characteristics of the study population and the prevalence of exclusive breastfeeding.
Bivariate and multivariate analysis were performed to examine the relationships between the independent variables and the dependent variable. In the bivariate analysis, chi-square tests were used to assess the associations between individual independent variables and the dependent variable. Following the bivariate analysis, logistic regression, was employed to examine the independent effects of multiple variables on exclusive breastfeeding.
Ethical approval and consent to participate
Ethical approval was obtained from the research ethics committee of SOS Community Nursing College (Ref: 2023/SOS-IRB/CNS/P005). Informed consent was also obtained from each participant, ensuring their privacy and confidentiality. Moreover, participation was voluntary, and participants had the right to withdraw at any time without consequences.
Result
Sociodemographic characteristics of the study participants
The findings of the study indicated that a significant proportion (55.9%) of the mothers interviewed fell within the age range of 20-30 years. Additionally, 34.5% of the respondents were older than 30 years, while 9.6% were below 20 years of age.
In terms of marital status, the study revealed that a substantial majority (84.3%) of the interviewed women were currently in a marriage contract, demonstrating a strong presence of married participants. Conversely, 15.7% of the women were either divorced or widowed.
In regard to education, a considerable percentage of both the interviewed women and their husbands lacked formal education, with approximately 56% of the women and 39% of the husbands falling into this category.
Furthermore, the study highlighted that a majority (73%) of the respondents were housewives, suggesting a high level of unemployment among the participants. Moreover, the majority (70.7%) of the respondents reported a monthly family income of less than 300 USD, indicating a prevalence of relatively low-income households within the studied population (Table 1).
Table 1. Socio-demographic characteristics of the respondents.| Variable | Frequency (N) | Percentage (%) |
|---|---|---|
| Maternal Age | ||
| Less than 20 years | 33 | 9.6 |
| 20-30 years | 193 | 55.9 |
| >30 years | 119 | 34.5 |
| Maternal Marital Status | ||
| Currently married | 291 | 84.3 |
| Currently not married | 54 | 15.7 |
| Marital status | ||
| Currently married | 291 | 84.3 |
| Currently not married | 54 | 15.7 |
| Maternal education | ||
| No formal education | 192 | 55.7 |
| Primary education | 64 | 18.6 |
| Secondary education | 53 | 15.4 |
| Post secondary education | 36 | 10.4 |
| Paternal education | ||
| No formal education | 135 | 39.1 |
| Primary education | 49 | 14.2 |
| Secondary education | 62 | 18.0 |
| Post secondary education | 99 | 28.7 |
| Maternal working status | ||
| Working | 94 | 27.2 |
| Not working | 251 | 72.8 |
| Monthly family income | ||
| <100USD | 69 | 20.0 |
| 100-299 USD | 175 | 50.7 |
| ≥300 USD | 101 | 29.3 |
Obstetric history and health service utilization
Of the 345 mothers who participated in the study, 181 (52.5%) of the mothers had more than three living children at the time of the study. The majority (62.3%) of the mothers at least attended ante natal care service once of whom 31% were given health education during the ANC visits.
However, 345 of the participants who took part in the study, 189 (54.8%) delivered in health facility while the remaining 45.2% delivered at homes. Similarly, 87.2% delivered through spontaneous vaginal delivery.
Regarding the child’s demographic characteristics, majority (81.4%) of the infants were born term, 55.9% females, 55.1% aged between 3-6 months and majority (66.1%) of them with preceding birth interval of <24 months. With respect to post-natal care, the majority (65.5%) of the respondents weren’t given post-natal counselling (Table 2).
Table 2. Obstetric history, child demographic characteristics and health service utilization| Variable | Frequency (N) | Percentage (%) |
|---|---|---|
| Parity | ||
| ≤3 | 164 | 47.5 |
| >3 | 181 | 52.5 |
| ANC attendance | ||
| Yes | 215 | 62.3 |
| No | 54 | 37.7 |
| ANC health education | ||
| Yes | 108 | 31.3 |
| No | 107 | 31.0 |
| NA | 130 | 37.7 |
| Place of delivery | ||
| Home | 156 | 45.2 |
| Health facility | 189 | 54.8 |
| Mode of delivery | ||
| Spontaneous vaginal delivery | 301 | 87.2 |
| Assisted/CS delivery | 44 | 12.8 |
| Gestational age at birth | ||
| Preterm | 28 | 8.2 |
| Term | 281 | 81.4 |
| Post term | 36 | 10.4 |
| Child sex | ||
| Male | 152 | 44.1 |
| Female | 193 | 55.9 |
| Child age | ||
| ≤ 3 months | 155 | 44.9 |
| >3 months | 190 | 55.1 |
| Preceding birth interval | ||
| NA | 54 | 15.7 |
| <24 months | 228 | 66.1 |
| >24 months | 63 | 18.3 |
| PNC Counselling | ||
| Yes | 119 | 34.5 |
| No | 226 | 65.5 |
Prevalence and patterns of child feeding
The study findings indicated that a majority (50%) of the interviewed mothers followed a mixed feeding practice, where their babies were fed with both breast milk and other types of milk. On the other hand, 44% of the mothers practiced exclusive breastfeeding, providing only breast milk to their infants. A smaller proportion (6%) of the mothers used cow's milk and infant formulas as feeding options for their babies (Figure 1). The study findings indicate that a mere 19% of mothers reported engaging in early breastfeeding initiation. This means that a relatively small proportion of the surveyed or studied mothers began breastfeeding their infants shortly after giving birth.
Figure 1.Distribution of child feeding patterns among children < 6 months
Reasons for not practicing exclusive breastfeeding
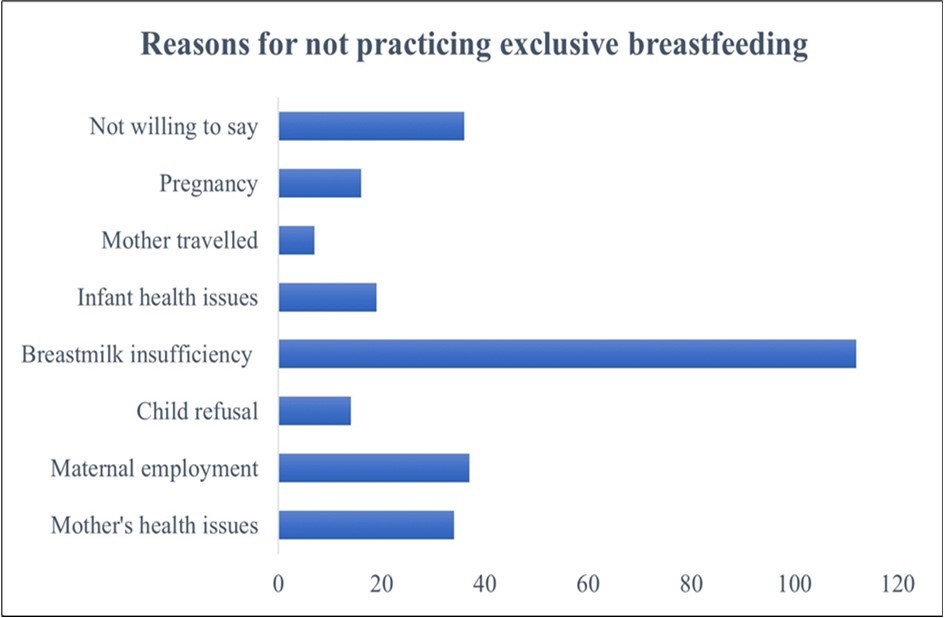
Inquiring about the factors contributing to the non-practice of exclusive breastfeeding, the primary reason cited by the majority of mothers was insufficient breast milk. Various factors such as perceived low milk supply and breastfeeding difficulties were attributed to this issue. The second most common reason mentioned was employment commitments, as mothers faced challenges in finding sufficient time for exclusive breastfeeding due to work obligations. Maternal and infant health issues also played a significant role, including medical conditions affecting breastfeeding or difficulties with infant latch and feeding. Pregnancy, particularly when occurring while breastfeeding, was another hindrance. Some mothers reported infant refusal of breastfeeding due to nipple confusion, discomfort, or alternative feeding preferences. Travel commitments were mentioned as well. It is noteworthy that some mothers chose not to disclose specific reasons, which could be personal or influenced by undisclosed factors. (Figure 2).
The Relationship Between Feeding Practices and the Incidence of Infant Illness
The study investigated the reported frequency of infant illness among mothers adopting different feeding practices, including exclusive breastfeeding, mixed feeding, and formula feeding. The findings revealed that among the interviewed mothers, only 3% of those practicing exclusive breastfeeding reported frequent infant sickness. In contrast, 25% of mothers using mixed feeding and a substantial 55% of those practicing formula feeding exclusively reported frequent illness in their infants. These results indicate a lower likelihood of infant sickness among breastfed infants, as reported by the participating mothers (Figure 3).
Figure 3.The relationship between feeding practices and infant sickness
Factors associated with exclusive breastfeeding practices
The study utilized binary logistic regression to investigate the relationship between exclusive breastfeeding and demographic, obstetric, and health service utilization factors. By employing this statistical analysis method, the researchers aimed to identify the specific factors that influence exclusive breastfeeding practices.
Demographic factors associated with exclusive breastfeeding practices
The results indicated that marital status, education level, and maternal working status were statistically significant factors in relation to exclusive breastfeeding. The findings revealed that mothers who were married had more than three times higher odds of practicing exclusive breastfeeding compared to those who were not married (adjusted odds ratio (AOR)=3.44, 95% confidence interval (CI): 1.559-7.598). Interestingly, the study found that education level had a somewhat unexpected impact on exclusive breastfeeding. Mothers with no formal education and those with primary education had approximately nine- and five-times higher odds, respectively, of practicing exclusive breastfeeding compared to those with post-secondary education. However, when it came to paternal education, the results differed. Babies whose fathers had secondary education were almost six times more likely to be breastfed compared to those whose fathers had no formal education (AOR=5.83, 95% CI: 2.555-13.312). Regarding maternal working status, the study revealed that housewives were about seven times more likely to practice exclusive breastfeeding compared to mothers who worked during the data collection period (AOR=6.77, 95% CI: 3.321-13.814).
In contrast to the other factors examined, the study did not find any significant association between exclusive breastfeeding and maternal age or income (Table 3).
Table 3. Demographic factors associated with exclusive breastfeeding among mothers having children aged 0–6 months old in Mogadishu, Somalia (n = 345)| Characteristics | N (%) | Exclusive breastfeeding | OR 95%(CI) | |||
| Yes=151 | No=194 | Crude odds ratio | Adjusted odds ratio | |||
| Maternal age | ||||||
|---|---|---|---|---|---|---|
| <20 years | 33(9.6) | 15(45.5) | 18(54.5) | 1 | 1 | |
| 20-30 years | 222(64.3) | 107(48.2) | 115(51.8) | 0.90(0.430-1.886) | 0.65(0.290-1.441) | |
| >30 years | 90(26.1) | 29(32.2) | 61(67.8) | 1.75(0.776-3.962) | 1.19(0.474-2.995) | |
| Marital status | ||||||
| Currently married | 291 (84.3) | 14 (19.7) | 92(29.4) | 3.20 (1.619-6.327) | 3.44(1.559-7.598) | |
| Currently not married | 54 (15.7) | 57 (80.3) | 221 (70.6) | 1 | 1 | |
| Maternal education | ||||||
| No formal education | 192(55.7) | 67 (34.9) | 125 (65.1) | 4.24 (1.966-9.146) | 8.62(3.138-23.667) | |
| Primary education | 64(43.8) | 28 (43.8) | 36 (56.3) | 2.92(1.231-6.934) | 4.50(1.565-12.957) | |
| Secondary education | 53(15.4) | 31(58.5) | 22(41.5) | 1.613(0.659-3.948) | 1.90(0.68-5.329) | |
| Post sec. education | 36(10.4) | 25(69.4) | 11(30.6) | 1 | 1 | |
| Paternal education | ||||||
| No formal education | 135(39.1) | 64 (47.4) | 71 (52.6) | 1 | 1 | |
| Primary education | 49(14.2) | 18 (36.7) | 31 (63.3) | 1.552(0.793-3.040) | 1.93(0.893-4.151) | |
| Secondary education | 62(18.0) | 16 (25.8) | 46 (74.2) | 2.592(1.337-5.022) | 5.83(2.555-13.312) | |
| Post sec. education | 99(28.7) | 53 (53.5) | 46 (46.5) | 0.782(0.465-1.316) | 1.16(0.799-3.266) | |
| Maternal working status | ||||||
| Working | 84 (24.3) | 17(20.2) | 67(79.8) | 1 | 1 | |
| Not working | 261 (75.7) | 134(51.3) | 127(48.7) | 4.16(2.317-7.464) | 6.77(3.321-13.814) | |
| Monthly family income | ||||||
| <100USD | 69 (20.0) | 31 (44.9) | 38 (55.1) | 1.11 (0.601-2.052) | 0.93(0.417-2.062) | |
| 100-299 USD | 175(50.7) | 72(41.1) | 103(58.9) | 1.30 (0.791-2.121) | 1.38(0.758-2.518) | |
| ≥300 USD | 101(29.3) | 48(47.5) | 53(52.5) | 1 | 1 | |
Obstetric and health service utilization factors associated with exclusive breastfeeding
The study focused on examining obstetric and health service utilization factors associated with exclusive breastfeeding. The results indicated significant associations between exclusive breastfeeding and three key factors: antenatal care (ANC) attendance, ANC health education, and postnatal care (PNC) counseling.
The study demonstrated that attending ANC sessions had a positive impact on exclusive breastfeeding. Mothers who attended at least one ANC appointment were nearly three times more likely to engage in exclusive breastfeeding compared to those who did not attend any ANC appointments (adjusted odds ratio (AOR)=2.89, 95% confidence interval (CI): 1.556-5.382). Regarding ANC health education, the findings revealed that mothers who received health education during ANC sessions had over 10 times higher odds of practicing exclusive breastfeeding compared to those who did not receive such education (AOR=10.42, 95% CI: 5.915-18.369).
Furthermore, the study found that postnatal counseling had a significant association with exclusive breastfeeding. Mothers who received counseling during the postnatal period were three times more likely to practice exclusive breastfeeding compared to those who did not receive any counseling (AOR=3.12, 95% CI: 1.64-5.928).
On the other hand, the study did not find any significant associations between exclusive breastfeeding and variables such as parity (number of previous births), place of birth, and mode of delivery (Table 4).
Table 4. Obstetric and health service utilization factors associated with exclusive breastfeeding among mothers having children aged 0–6 months old in Mogadishu, Somalia (n = 345)| Characteristics | N (%) | Exclusive breastfeeding | OR 95%(CI) | ||
| Yes=151 | No=194 | Crude odds ratio | Adjusted odds ratio | ||
| Parity | |||||
|---|---|---|---|---|---|
| ≤3 | 164 (47.5) | 82 (50.0) | 82(50.0) | 1.62(1.057-2.492) | 1.45(0.831-2.530) |
| >3 | 181 (52.5) | 69(38.1) | 112(61.9) | 1 | 1 |
| ANC attendance | |||||
| Yes | 215 (62.3) | 126(58.6) | 89(41.4) | 5.95(3.557-9.939) | 2.89(1.556-5.382) |
| No | 130 (37.7) | 25(19.2) | 105(80.8) | 1 | 1 |
| ANC health education | |||||
| Yes | 135(31.3) | 106(78.5) | 29(21.5) | 13.40(7.915-22.693) | 10.42(5.915-18.369) |
| No | 210(68.7) | 45(21.4) | 165(78.6) | 1 | 1 |
| Place of delivery | |||||
| Home | 156 (45.2) | 81(51.9) | 75(48.1) | 1 | |
| Health facility | 189 (54.8) | 70 (37.0) | 119 (63.0) | 1.84(1.193-2.825) | 1.33(0.710-2.473) |
| Mode of delivery | |||||
| SV delivery | 301 (87.2) | 128(42.5) | 173(57.5) | 1.48(0.785-2.791) | 1.32(0.510-3.464) |
| CS delivery | 44 (12.8) | 23 (52.3) | 21 (47.7) | 1 | 1 |
| PNC Counselling | |||||
| Yes | 119(34.5) | 78(65.5) | 41(34.5) | 4.00(2.493-6.378) | 3.12(1.64-5.928) |
| No | 226(65.5) | 73(32.3) | 153(67.7) | 1 | 1 |
Baby-related factors associated with exclusive breastfeeding
With respect to the baby-related factors, the study revealed that child sex and child age. Male babies had almost three times odd for exclusive breastfeeding compared to female babies (AOR=2.74, 95%CI:1.736-4.314). Similarly, children whose age is below 3 months of age had 1.6 odds for exclusive breastfeeding compared to those older than 3 months of age (AOR=1.62, 95%CI:1.023-2.547) (Table 5).
Table 5. Baby-related factors associated with exclusive breastfeeding among mothers having children aged 0–6 months old in Mogadishu, Somalia (n = 345)| Characteristics | N (%) | Exclusive breastfeeding | OR 95%(CI) | ||
| Yes=151 | No=194 | Crude odds ratio | Adjusted odds ratio | ||
| Gestational age at delivery | |||||
| Preterm/Post term | 64 (15.6) | 20(31.3) | 44(68.7) | 1.92(1.078-3.425) | 1.76(0.964-3.196) |
| Term | 281 (81.4) | 151(43.8) | 194(56.2) | 1 | 1 |
| Child sex | |||||
| Male | 170 (49.3) | 95(55.9) | 75(44.1) | 2.70(1.736-4.174) | 2.74(1.736-4.314) |
| Female | 175 (50.7) | 56(32.0) | 119 (68.0) | 1 | 1 |
| Child age | |||||
|---|---|---|---|---|---|
| ≤ 3 months | 155 (44.9) | 75(48.4) | 80(51.6) | 1.41(0.916-2.158) | 1.62(1.023-2.547) |
| >3 months | 190(55.1) | 76(40.0) | 114 (60.0) | 1 | 1 |
Discussion
Breastfeeding goes beyond being a mere choice of lifestyle; it is a valuable investment in the realm of health. It offers unparalleled advantages for both infants and mothers. Babies who receive breast milk experience decreased chances of developing asthma, obesity, Type 1 diabetes, severe lower respiratory disease, acute otitis media, sudden infant death syndrome, gastrointestinal infections, and necrotizing enterocolitis in the case of preterm infants13, 14. The WHO and the United Nations Children's Fund (UNICEF) recommend that children be exclusively breastfed for the first 6 months of life—meaning no other foods or liquids are provided, including water13.
In this study, the prevalence of exclusive breastfeeding was found to be 44%. Although this rate is slightly higher than the general prevalence of exclusive breastfeeding in the country15, it is still lower than the rates reported in neighboring countries16, 17. Among the remaining 56% of mothers, 50% engage in mixed feeding practices, which involve the combination of breastmilk and animal milks. On the other hand, approximately 6% of the mothers exclusively rely on cow's milk and infant formulas as feeding options for their babies.
The study has uncovered several factors linked to the practice of exclusive breastfeeding. In terms of demographic characteristics, the findings of the study demonstrated that marital status, educational attainment, and maternal employment were statistically significant factors associated with exclusive breastfeeding.
The results indicated that married mothers had over three times greater likelihood of engaging in exclusive breastfeeding in comparison to unmarried mothers. Similarly, a study conducted in Ethiopia yielded comparable results. Just like our findings, the study in Ethiopia also revealed a higher prevalence of exclusive breastfeeding among married mothers. This consistent pattern suggests that marital status may be an influential factor in promoting exclusive breastfeeding practices18.
Surprisingly, the study discovered an intriguing relationship between education level and exclusive breastfeeding. Contrary to various studies conducted in Africa and Asia 19, 20, 21, 22, our findings revealed that mothers with no formal education had around nine times higher odds of practicing exclusive breastfeeding, while those with primary education had approximately five times higher odds in comparison with university graduates. Almost similar result was reported by Hossain et al23. This deviation from previous research highlights a unique perspective on the impact of education on exclusive breastfeeding practices. This disparity could potentially be attributed to multiple factors. One possible explanation is that mothers with university education often have demanding jobs that require regular attendance, making it challenging to exclusively breastfeed their infants.
Contrastingly, the results showed a divergence in the influence of paternal education. Infants whose fathers had received formal education exhibited nearly six times higher odds of being breastfed in comparison to those whose fathers had no formal education. This finding aligns with the results of a controlled randomized trial conducted in Iran. The study conducted in Iran reported similar outcomes, reinforcing the notion that paternal education plays a significant role in promoting breastfeeding practices24. This can be attributed to the influential role that fathers play in decision-making regarding the mode of feeding for their child.
In terms of maternal employment status, the study findings indicated that housewives had approximately seven times higher odds of practicing exclusive breastfeeding compared to mothers who were employed. Consistent findings have been reported by several studies conducted in various countries and settings. These studies have also reported similar trends and associations, further strengthening the evidence regarding the impact of maternal employment on exclusive breastfeeding practices25, 26, 27.
In addition to demographic characteristics, the study revealed that obstetric and health service utilization factors were also associated with exclusive breastfeeding. Specifically, significant associations were found between exclusive breastfeeding and three key factors: attendance of antenatal care (ANC), receipt of ANC health education, and postnatal care (PNC) counseling.
Mothers who attended at least one ANC appointment were nearly three times more likely to engage in exclusive breastfeeding compared to those who did not attend any ANC appointments. This finding is consistent with the results of another study conducted in India, which also demonstrated similar outcomes28. This can be attributed to the fact that during antenatal care (ANC) visits, mothers receive education and information regarding the significance of exclusive breastfeeding. The counseling and educational sessions provided during ANC visits likely contribute to the increased awareness and understanding among mothers about the benefits and importance of exclusive breastfeeding.
The study revealed an important finding regarding the impact of health education during ANC visits on exclusive breastfeeding practices. It was observed that ANC visits with health education sessions had over 10 times higher odds of practicing exclusive breastfeeding compared to visits without such sessions. The observed association can be attributed to the positive impact of health education talks provided during ANC visits. These informative sessions contribute to raising awareness and promoting the practice of exclusive breastfeeding among mothers. Similar studies have consistently reported comparable findings, further corroborating the obtained results29, 30, 31.
Postnatal counseling emerged as another significant factor influencing exclusive breastfeeding practices. The study revealed that mothers who received counseling during the postnatal period were three times more likely to engage in exclusive breastfeeding compared to those who did not receive any postnatal care (PNC) counseling. A comparable study yielded comparable results, further strengthening the findings of the current study32.
The study uncovered noteworthy findings related to baby-related factors and their association with exclusive breastfeeding. Specifically, child sex and age were identified as statistically significant factors. Male babies were found to have nearly three times higher odds of exclusive breastfeeding compared to female babies. This observation may be attributed to cultural preferences among Somali families, where there is a tendency to prioritize male babies over female babies.
Likewise, the study revealed a similar pattern with regards to the age of the children. Infants below the age of 3 months were found to have 1.6 times higher odds of practicing exclusive breastfeeding compared to those who were older than 3 months. This finding underscores the importance of early initiation of exclusive breastfeeding and the potential decline in exclusive breastfeeding rates as infants grow older. This finding is in line with the results of a separate study conducted in neighboring Ethiopia, which also indicated a decrease in exclusive breastfeeding with increasing age of the child33. This can be attributed to several factors. As the child's age increases, some mothers may perceive breast milk as insufficient to meet the growing nutritional needs of their child, leading them to introduce supplementary feeds.
In relation to infants' health status and exclusive breastfeeding, the study revealed that mothers who exclusively breastfed their infants reported a significantly lower frequency of infant sickness (3%) compared to mothers who practiced mixed feeding (25%) or formula feeding (55%). Similar findings have been reported by other studies conducted in different settings, further supporting the association between exclusive breastfeeding and a lower frequency of infant sickness. These studies have consistently shown that infants who are exclusively breastfed have a reduced risk of various infections, respiratory illnesses, gastrointestinal disorders, and other health-related issues34, 35. The lower frequency of infant sickness reported among mothers practicing exclusive breastfeeding can be attributed to the unique composition of breast milk, which provides optimal nutrition and essential antibodies that help boost the infant's immune system.
Strength and limitations
The study demonstrated several strengths in its methodology. Firstly, the researchers used the Kish and Leslie formula to determine a representative sample size of mothers with infants under six months attending SOS Mother and Child Hospital in Mogadishu. This ensures that the study participants are a reliable representation of the target population. Additionally, the collected data underwent rigorous checks for accuracy, completeness, and consistency. Through data cleaning procedures, any missing or erroneous data points were addressed, further enhancing the reliability of the study's findings. Furthermore, logistic regression analysis was employed to examine the independent effects of multiple variables on exclusive breastfeeding. This statistical approach allowed for the identification of significant factors associated with exclusive breastfeeding, considering the influence of various variable simultaneously. These strengths collectively contribute to the study's reliability and comprehensive understanding of the determinants of exclusive breastfeeding in the study population.
On the other hand, the study does have some limitations. Firstly, it was conducted exclusively among mothers seeking healthcare services at SOS Mother and Child Hospital in Mogadishu, which may limit the generalizability of the findings to a broader population of mothers with infants in Mogadishu or other regions of Somalia. Secondly, the study's cross-sectional design only provides a snapshot of the prevalence and determinants of exclusive breastfeeding at a specific point in time. This design does not allow for establishing causality or examining changes in breastfeeding practices over time. These limitations should be taken into consideration when interpreting the results and applying them to a wider context.
Conclusion
The findings of this study highlight the significant benefits of exclusive breastfeeding for both infants and mothers. It emphasizes that breastfeeding is not merely a lifestyle choice but a crucial investment in the realm of health. Infants who receive breast milk experience lower risks of developing various illnesses and conditions, ranging from respiratory diseases to gastrointestinal infections. The prevalence of exclusive breastfeeding in the study population was 44%, slightly higher than the general prevalence in the country but lower than rates reported in neighboring countries. Several factors were identified as influencing exclusive breastfeeding practices, including marital status, maternal education, paternal education, maternal employment, and utilization of antenatal and postnatal care services. The study also underscored the importance of health education during antenatal care visits and postnatal counseling in promoting exclusive breastfeeding. Furthermore, baby-related factors such as child sex and age were found to be associated with exclusive breastfeeding. Male infants and younger infants had higher odds of being exclusively breastfed. The study also revealed a significant correlation between exclusive breastfeeding and a lower frequency of infant sickness, further supporting the health benefits of breastfeeding.
Recommendation
Based on the research findings, it is recommended to prioritize and promote exclusive breastfeeding as the optimal feeding practice for infants. Efforts should be directed towards raising awareness among mothers and families about the numerous health advantages of exclusive breastfeeding. Antenatal care visits should include comprehensive health education sessions that emphasize the importance and techniques of exclusive breastfeeding. Additionally, postnatal counseling should be provided to mothers to support and encourage exclusive breastfeeding practices. Health institutions and policymakers should develop and implement supportive policies and programs that facilitate exclusive breastfeeding, particularly for working mothers. Maternity leave policies should be designed to allow sufficient time for exclusive breastfeeding and to promote successful initiation and continuation of breastfeeding. Community-based initiatives and support groups can play a significant role in providing guidance, counseling, and peer support for mothers in their breastfeeding journey. It is essential to address cultural beliefs and practices that may discourage or hinder exclusive breastfeeding, and to foster a supportive environment that promotes breastfeeding as the norm.
Funding information
This work received no funding.
Data availability statement
Data will be made accessible upon a reasonable request to the corresponding author.
Declaration of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
We express our gratitude to the interviewers (020) for their helpful support and time, as well as to the participants who willingly took part in our study.
References
- 1.Dieterich C M, Felice J P, O’Sullivan E, Rasmussen K M. (2013) Breastfeeding and Health Outcomes for the Mother-Infant Dyad. Pediatric clinics of North America. Feb;60(1): 31.
- 2. (2023) Infant-feeding practices and their relationship with diarrheal and other diseases in Huascar (Lima). PubMed [Internet]. [cited , Peru
- 3.Alimoradi F, Javadi M, Barikani A, Kalantari N, Ahmadi M. (2014) An Overview of Importance of Breastfeeding. , Journal of Comprehensive Pediatrics 5(2), 14028.
- 4.Gill S L, Reifsnider E, Lucke J F, Mann A R. (2007) Predicting breast-feeding attrition: Adapting the breast-feeding attrition prediction tool. , Journal of Perinatal and Neonatal 21(3), 216-24.
- 5.Lönnerdal B. (2000) Breast milk: a truly functional food. Nutrition. Jul;16(7–8): , (Burbank, Los Angeles County, Calif) 509-11.
- 6.Edmond K M, Zandoh C, Quigley M A, Amenga-Etego S, Owusu-Agyei S et al. (2006) Delayed Breastfeeding Initiation Increases Risk of Neonatal Mortality. Pediatrics. 117(3), 80-6.
- 7.César J A, Victora C G, Barros F C, Santos I S, Flores J A. (1999) Impact of breast feeding on admission for pneumonia during postneonatal period in Brazil: nested case-control study. BMJ (Clinical research ed). 318(7194), 1316-20.
- 8.Sharma D, Hanson L, Korotkova M, Telemo E, Ogra P. (2015) Human Milk: Its Components and Their Immunobiologic Functions. Mucosal Immunology: Fourth Edition. 1, 2307-41.
- 9.Ejie I L, Eleje G U, Chibuzor M T, Anetoh M U, Nduka I J et al. (2021) A systematic review of qualitative research on barriers and facilitators to exclusive breastfeeding practice in sub-Saharan African countries. International Breastfeeding Journal. 16(1), 1-13.
- 10.JPC Dukuzumuremyi, Acheampong K, Abesig J, Luo J Knowledge. (2020) attitude, and practice of exclusive breastfeeding among mothers in East Africa: A systematic review. International Breastfeeding Journal. 15(1), 1-17.
- 11.EMRO WHO. (2023) Government of Somalia, UNICEF and WHO mark World Breastfeeding Week with a call to step up breastfeeding-friendly environments for mothers and babies | News | Somalia site [Internet]. [cited. Available from: https://www.emro.who.int/somalia/news/government-of-somalia-unicef-and-who-mark-world-breastfeeding-week-with-a-call-to-step-up-breastfeeding-friendly-environments-for-mothers-and-babies.html
- 12.sampling Survey. (2023) by Leslie Kish | Open Library [Internet]. [cited. Available from: https://openlibrary.org/books/OL5947497M/Survey_sampling
- 13. (2023) Infant and young child feeding [Internet]. [cited. Available from: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding
- 15.Women Somalia’s. (2023) and Children are Among the 1.84 Million to Benefit from Improved Healthcare Services [Internet]. [cited. 2021-07.
- 16. (2023) Exclusive breastfeeding (% of children under 6 months) - Kenya | Data [Internet]. [cited. Available from: https://data.worldbank.org/indicator/SH.STA.BFED.ZS?locations=KE
- 17.Wake G E, Mittiku Y M. (2021) Prevalence of exclusive breastfeeding practice and its association with maternal employment in Ethiopia: a systematic review and meta-analysis. International Breastfeeding Journal. 16(1), 1-14.
- 18.Muluneh M W. (2023) Determinants of exclusive breastfeeding practices among mothers in Ethiopia. PLOS ONE.
- 19.Edmond K M, Zandoh C, Quigley M A, Amenga-Etego S, Owusu-Agyei S et al. (2006) Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics.
- 20.Onah S, DIC Osuorah, Ebenebe J, Ezechukwu C, Ekwochi U et al. (2014) Infant feeding practices and maternal socio-demographic factors that influence practice of exclusive breastfeeding among mothers in Nnewi South-East Nigeria: a cross-sectional and analytical study. International Breastfeeding Journal. 6.
- 21.Knowledge. (2016) attitudes and determinants of exclusive breastfeeding practice among Ghanaian rural lactating mothers. International Breastfeeding Journal. 11(1), 1-8.
- 22.Sarkar P, Rifat M A, Bakshi P, Talukdar I H, SML Pechtl et al. (2023) How is parental education associated with infant and young child feeding in Bangladesh? a systematic literature review. BMC Public Health. 23(1), 1-35.
- 23.Hossain M, Islam A, Kamarul T, Hossain G. (2018) Exclusive breastfeeding practice during first six months of an infant’s life in Bangladesh: A country based cross-sectional study. BMC Pediatrics. 18(1), 1-9.
- 24.Panahi F, Rashidi Fakari F, Nazarpour S, Lotfi R, Rahimizadeh M et al. (2022) Educating fathers to improve exclusive breastfeeding practices: a randomized controlled trial. BMC Health Services Research. 22(1), 1-12.
- 25.Ahmmed F, Hossain M J, Sutopa T S, Al-Mamun M, Alam M et al. (2022) The trend in exclusive breastfeeding practice and its association with maternal employment in Bangladesh: A multilevel analysis. Frontiers in Public Health. 25, 988016.
- 26.Santos M N, Azeredo C M, AEM Rinaldi. (2022) Association Between Maternal Work and Exclusive Breastfeeding. in Countries of Latin America and Caribbean. Maternal and Child Health Journal 26(7), 1496-506.
- 27.Tadesse F, Alemayehu Y, Shine S, Asresahegn H, Tadesse T. (2019) Exclusive breastfeeding and maternal employment among mothers of infants from three to five months old in the Fafan zone, Somali regional state of Ethiopia: A comparative cross-sectional study. BMC Public Health. 19(1), 1-9.
- 28.Tiwari R, Mahajan P C, Lahariya C. (2009) The Determinants of Exclusive Breast Feeding in Urban Slums: A Community Based Study. Journal of Tropical Pediatrics. 55(1), 49-54.
- 29.Ogbo F A, Agho K E, Page A. (2015) Determinants of suboptimal breastfeeding practices in Nigeria: Evidence from the 2008 demographic and health survey. BMC Public Health. 15(1), 1-12.
- 30.Ogbo F A, Dhami M V, Awosemo A O, Olusanya B O, Olusanya J et al. (2019) Regional prevalence and determinants of exclusive breastfeeding in India. , International Breastfeeding Journal. May 14(1), 1-12.
- 31.Dahie H A. (2022) Determinants of maternal near miss events among women admitted to tertiary hospitals in Mogadishu, Somalia: a facility-based case–control study. BMC Pregnancy and Childbirth.
- 32.Mamo K, Dengia T, Abubeker A, Girmaye E.Assessment of Exclusive Breastfeeding Practice and Associated Factors among Mothers in West Shoa Zone. Obstetrics and Gynecology International , Oromia, Ethiopia 2020-2020.
- 33.Alemayehu T, Haidar J, Habte D. (2009) Determinants of exclusive breastfeeding practices in Ethiopia. Ethiopian Journal of Health Development. 23(1), 12-8.