Giant Ileal Conduit Stone: Feasibility of Endoscopic Lithotripsy: A Case Report and Review of Literature
Abstract
Ileal conduit has been considered the urinary diversion of choice following radical cystectomy although orthotopic bladder substitution is gaining popularity. Urinary diversions are associated with complications including stone formation in up to 54%.
We report the management of the largest ileal conduit stone reported in the literature.
Author Contributions
Academic Editor: Andreas Bourdoumis, Mr Andreas Bourdoumis, MD,PhD, FEBU, FES Consultant Urological Surgeon Acute Pennine Hospitals NHS Trust Manchester, UK, Email: [email protected]
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Ala’a Sharaf, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Ileal conduit (IC) has been considered the urinary diversion of choice following radical cystectomy although orthotopic bladder substitution is gaining popularity1, 2. Urinary diversions are associated with complications including stone formation in up to 54% due to various reasons such as urinary stasis, mucus formation, suture nidus and bacteriuria3. Various techniques have been applied in the treatment of Ileal conduit stones via an open or minimally invasive access. In this study we report the management of the largest ileal conduit stone reported in the literature.
Case Report
We report a case of a gentleman with spina bifida who underwent urinary diversion in the form of an ileal conduit as a child and presented 40 years later with worsening renal function that was picked up by his general practioner during routing investigations. Clinical examination revealed a hard mass superomedial to the right parararectal stoma. An initial ultrasound scan showed bilateral hydronephrosis and a possible calculus in the conduit. A subsequent CT KUB showed a 13 cm x 4 cm calculus occupying most of the conduit causing outflow obstruction (Figure 1). He also had a 2cm left renal calculus. Following a Foley catheter insertion into the stoma under image guidance, his renal function returned to normality. The patient was counselled for both the open and endoscopic approach.
Under a general anaesthetic, the patient was in prone position and given prophylactic co-amoxiclav. A 30f nephroscope was inserted into the stoma and a large calculus encountered (Figure 2). Using lithoclast probes, calculus was broken into smaller fragments and extracted using forceps. A Foley catheter balloon was inflated proximal to the calculus to prevent reflux of small fragments into the kidney (Figure 3). Total operation time was 210 minutes with no blood loss and the patient required 5mg of morphine throughout the procedure.
Figure 2.Nephroscopy in the conduit
Figure 3.Conduit stone fragments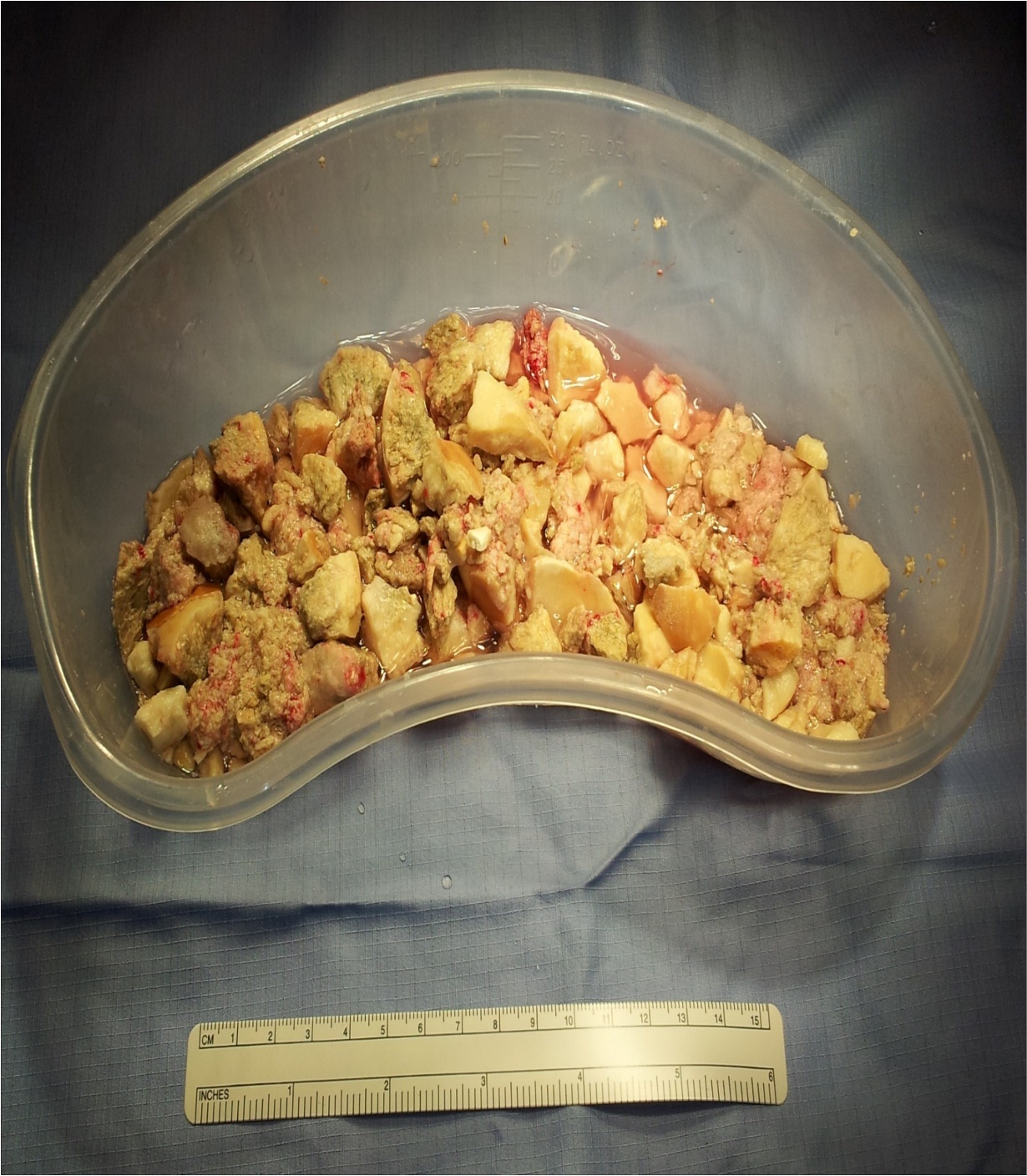
A post operative CT KUB confirmed complete clearance of the ileal conduit calculus and return of normal baseline renal function (Figure 4). He had no post operative complications and the ilial conduit was functioning normally and no urinary drainage was required. The patient was discharged the following day with no issues.
Figure 4.Post-operative CT scan revealing a stone free ileal conduit.
Discussion
Majority of patients with IC do have long term favourable results. Complications occur in approximately in 54% of patients3, 4. Early complications include urinary leak at the uretero-ileal anastomosis (7-14%), paralytic ileus (18-22%) and bowel obstruction (5-10%). Late complications include Uretero-ileal anastomotic strictures (4-7%), pouch stone formation (10%-50%), parastomal hernia (10-15%) and stomal prolapse (1.5-8%) 1, 3.
Most urolithiasis reported in the literature appears to present in the upper tracts rather than the conduit 5, 6. However, IC stones have been reported on a number of occasions. Topuzovic et al7reported a 10cm ileal conduit stone which was treated by using a Kocher forceps and grasping the stone then removing it intact from the IC. This resulted in minimal bleeding which was controlled with intraoperative irrigation and the patient was discharged the following day. Gomez Pascual et al8 reported a 15x10 cm IC stone which was extracted after a laparotomy.
Urolithiasis in a patient with IC is amenable to commonly utilised management strategies such as extra corporeal shock wave lithotripsy (ESWL), ureteroscopy, percutaneous endoscopic surgery as well as open or laparoscopic surgery4. Management depends on the size and composition of the stone, anatomy of the conduit and general condition of the patient. Although ESWL can be used in both continent and incontinent urinary diversion, given the dependency of the IC and sluggish drainage expulsion of stone fragments is difficult. Hence endoscopic approaches with active removal of fragments may provide long term calculus clearance. For large calculi open techniques have been employed as a way of achieving complete clearance.
In our case, the decision to perform endoscopic procedure was taken because we felt that to violate a well-functioning 30-year-old conduit with its attendant complications was too high a risk. We felt that complications will be minimized if we can complete the procedure endoscopically. Although it had taken 210 minutes for the whole procedure, the patient was ambulant the same day and only required simple analgesia post operatively. We suggest that where feasible endoscopic approach offers less invasive option for the treatment of ileal conduit stones.
References
- 2.Colombo R, Naspro R. (2010) Ileal conduit as the standard for urinary diversion after radical cystectomy for bladder cancer. , European Urology, Supplements 9, 736-744.
- 3.Farnham S B, Cookson M S. (2004) Surgical complications of urinary diversion. , World J Urol; 22(3), 157-167.
- 4.Hertzig L L, Iwaszko M R, Rangel L J, Patterson D E, Gettman M T et al. (2013) Urolithiasis after ileal conduit urinary diversion: a comparison of minimally invasive therapies. , J Urol; 189(6), 2152-2157.
- 5.Madersbacher S, Schmidt J, Eberle J M. (2003) Long-term outcome of ileal conduit diversion. , J Urol; 169(3), 985-990.
- 6.Turk T M, Koleski F C, Albala D M. (1999) Incidence of urolithiasis in cystectomy patients after intestinal conduit or continent urinary diversion. , World J Urol; 17(5), 305-307.

