Inferior Turbinate Surgery: Difficulties Between the Decision-Making and the Selection of Proper Technique
Abstract
Back ground and Objectives
The inferior conchae have important role in the maintenance of nasal airflow via providing the nasal valve mechanism but increase of inferior turbinate bulk may result in significant nasal obstruction. Therefore, this may need further surgical intervention to deal with these bulky conchae but it is very necessary to balance between the mechanical as well as the functional patency of the nose. Thus, through this surgery it become difficult to decide whether the patient is a candidate for surgery and which technique is suitable for that particular patient.
Patients and Methods
Two- thousands three- hundreds and six patients aged 3-65 years of hypertrophied inferior conchae, had been diagnosed as a cases of mechanical nasal obstruction due to hypertrophied inferior conchae (HIC). The patients operated by two techniques of inferior conchae surgery, which are sub-mucosal diathermy (SMD) and partial inferior turbinectomy (PIT). The outcomes were correlated to different factors to assess as much as possible the clear conclusion for this significant issue in rhinology.
Results and Conclusion
The proper selection of patient for this pattern of surgery is considered as one of main aspects of this issue and one of significant steps toward the resolving of this dilemma it is very necessary to select the most suitable candidate for this surgery. On the other hand, the type of the technique for this surgery is needed to be selected probably.
Author Contributions
Academic Editor: I Beegun, London North Thames ENT.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Khaled Mohamed Bofares
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The inferior concha surgery is one of common surgeries in rhinology. Simply it is performed by the reduction of the size of inferior conchae to treat the mechanical nasal obstruction due to hypertrophied inferior conchae. The reduction of the size of the inferior conchae should not done randomly. This is important to preserve the eddy current flow of the air into the nose by maintaining the inferior conchae valve mechanism thus from this view, the clinical studies are frequently conducted just mainly to achieve the aim how to maintain the balance between the mechanical and the functional obstruction 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20.
Hence, the sufficient size of inferior conchae is important to maintain normal nasal breathing function. In the same time, the hypertrophied inferior conchae (HIC) that occupy more than one-third of nasal cavity may be presented with significant nasal obstruction related symptomology. Thus the main aim of the inferior conchae surgery is the balancing in between the over-resection and under-resection of inferior turbinate at optimum level that provide the preservation of sufficient breathing function through the nose in addition to relieving the mechanical obstruction due to inferior conchae hypertrophy 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 33, 34, 35.
The etiologies of inferior conchae hypertrophy could be allergic rhinitis, vasomotor rhinitis, chronic hypertrophic rhinitis, rhinitis medica-mentosa and chronic infective rhinitis as fungal rhinitis. All these conditions can be treated and controlled probably by medical treatment before the decision of any surgical interventions. The size and the contour of inferior conchae are needed for keeping of normal nasal ventilation function therefore the medical therapy for inferior conchae hypertrophy still is considered as the cornerstone of management before the surgery 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35.
In accordance, the inferior conchae surgery can be done for relieving of mechanical nasal obstruction due to confirmed persistent inferior conchae hypertrophy, for achievement a sufficient surgical access, and as a part of wide resection procedures 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35.
Throughout, the last century and the presenting century as one of progressing parts in the rhinology is the inferior conchae surgery. Indeed, there are many patterns of this surgery were conducted as submucosal diathermy, partial inferior turbinectomy, CO2 laser vaporization, Argon laser vaporization, turbinoplasty, and lateral nasal wall lateralization. Each of these modalities has advantages and disadvantages, which need to be correlated with each patient who had been, decided as a candidate for inferior conchae surgery.
Hence, sometimes, there will be certain difficulties that may interfere with the proper selection of most suitable modality for each particular patient. Subsequently, the achieved sequels of this surgery will not be as predicted therefore this type of surgery was considered as one of difficult surgeries in rhinology 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35.
Thus, this serial clinical trial was proposed as prospective analytic study to highlight as much as possible these difficulties. The main aims of this study were based on the answer of these questions:
1. What are the criteria of the patient that can be considered as most suitable patient for this surgery?
2. Which pattern of this procedure will be decided as most proper technique for this particular patient?
3. How much the size of inferior concha is required to be removed?
4. and as a idea to maintain the proper size and contour of inferior turbinate, is it needed to do concomitant septoplasty with inferior conchae surgery or not?
Patients and Methods
Two- thousands three- hundreds and six patients aged 3-65 years of persistent inferior conchae hypertrophy associated with different etiologies namely allergic rhinitis, and vasomotor rhinitis, presented with mechanical nasal obstruction that not responding to sufficient medical treatment at ENT department – Althowra central hospital and Altarahom private center – Elbyda city – Libya at period in between September 2005 to June 2021. The patients operated by different two of inferior turbinate surgery, namely sub-mucosal diathermy (SMD) (n=1550) and partial inferior turbinectomy (PIT) (n=756). SMD group was divided in relation to conducted cauterization points into three sub-groups (two points sub-group, three points sub-group, and four points sub-group). In addition, PIT group was classified according to the amount of resected tissue into three sub-groups too. Sub-group-A, that include those patients who underwent for the resection of one-third of HIC, sub-group-B, that include those patients who underwent for the resection of two-thirds of HIC, and sub-group-C, that include those patients who underwent for the subtotal resection of HIC). On the other hand, the part of patients who interfered with SMD and PIT were operated concomitantly with septoplasty (n= 638, n= 313 consecutively), and compared to those who operated by solitary SMD and PIT (n= 912, n= 443 consecutively) to assess the effect of concomitant septoplasty on outcomes of inferior conchae surgery. The outcomes of the surgery were correlated to different patients' demographic, environmental, habitual, socio-economic, pathological as well as technical factors. Postoperatively, all the patients were assessed throughout first week for any nasal bleeding and followed up for 3-36 months for common late complications of the surgery such as the persistence or recurrence of mechanical nasal obstruction, and post-operative atrophic rhinitis. The nasal obstruction was assessed by elucidation of any olfactory impairment in addition to application of cottle's test and atrophic rhinitis was diagnosed clinically by recognition of local atrophic changes.
Economically speaking, the expense of each technique was evaluated in relation to drugs consumption. This was including anesthesia drugs, systemic antibiotics, analgesic drugs, intravenous fluids, post-operative local irrigation solutions, and sometimes-anticoagulant drugs as tranxiemic acid. In addition, local nasal packs, expense related to patient's word admission, and by the end, the expense related to patient post-operative follow-up. An informed consent was taken from the patients involved in the research prior to their participation.
Data were expressed by using descriptive analysis as means + standard error of mean (s. e. m) and percentages, test of significance was carried out, using Chi-square test and two way analysis of variance. A probability less than 0.05 was considered as significant, the degree of significance was determined by using level of standard deviation test. Student -t- test was used for dependent sample, as well as contingency coefficient was calculated as measurement of association between nominal variables.
Results
As shown in (Figure 1, Figure 2) the incidence of post-operative epistaxis and atrophic rhinitis was correlated to two significant factors which are the age of patient and the type of performed technique. It was found that the PIT increased significantly the risk of post-operative bleeding and atrophic rhinitis up to (20%) and (35%) consecutively among elderly patients as compared to SMD (P < 0.05). On the other hand, as illustrated in (Figure 3) the incidence of post-operative recurrence of HIC was correlated to the patient related environmental and habitual factors. It was found that SMD is associated with higher percentage of recurrence (30%) as compared to PIT among heavy smoking patients as well as the patients with history of usual exposure to allergic rhinitis inducing allergens (P < 0.05). In accordance the (Table 1) elucidate the effect of patients' local health status on outcomes of the inferior concha surgery, it was found that the patients with allergic rhinitis and vasomotor rhinitis who operated by PIT showed a significant long-standing improvement may reach up to 93% as compared to those who interfered by SMD (P < 0.05). As demonstrated in (Table 2) the effect of patients' general health status in relation to the type of performed procedure. It was confirmed that the patients with uncontrolled systemic hypertension had a significant raising in the risk of post-operative epistaxis after PIT as compared to SMD and those patients with uncontrolled diabetes mellitus shown higher risk of recurrence of nasal obstruction after SMD as compared to PIT (P < 0.05). On the other hand, (Figure 4) was elucidated the comparison between two techniques in relation to operative time consumption, it was found that the duration of PIT was significantly longer as compared to SMD (P < 0.05). Therefore from economic point of view, as illustrated at (Table 3) PIT can be classified significantly with higher expense as compared to SMD (P < 0.05). From other side, as can be seen from (Table 4) the amount of direct or indirect reduction of inferior conchae size had a significant effect on outcomes of the performed procedure. As it is presented at the same table these results was correlated with number of cauterization points in SMD, and the resected size of inferior concha in PIT. On the other hand there was significant improvement for outcomes of SMD and PIT if they are performed concomitantly with septoplasty procedure (P < 0.05).
Figure 1.The incidence of post-operative epistaxis (percentage) in relation to patients' age and type of procedure (P < 0.05).
Figure 2.The incidence of post-operative atrophic rhinitis (percentage) in relation to patients' age and type of procedure (P < 0.05).
Figure 3.The incidence of recurrence of HIC (%) in correlation with the patient related environmental and habitual factors (P < 0.05).
Figure 4.The comparison between PIT and SMD in relation to intraoperative time consumption in minutes (P < 0.05).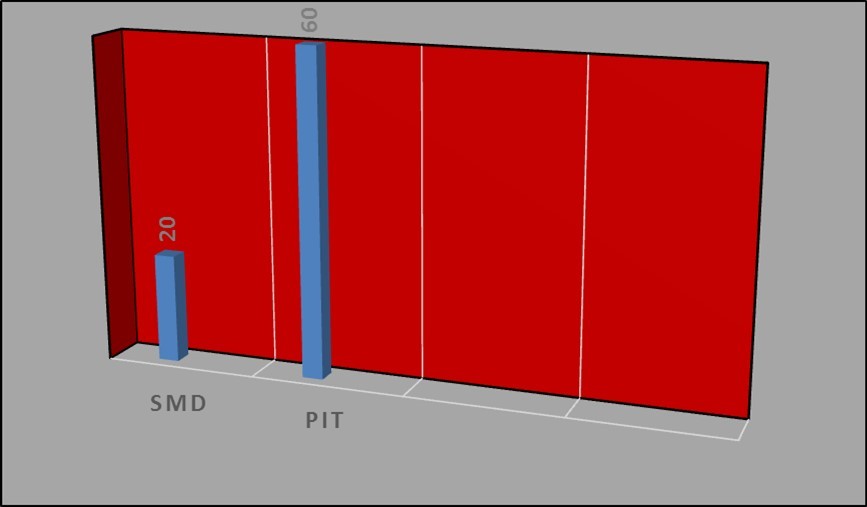
| Type of local pathology | Percentage (%) of persistence of nasal patency improvement for 36 months in relation to type of procedure | ||
|---|---|---|---|
| SMD (N=1550)(ARn= 930 & VMRn =620) | PIT (N=756)(ARn= 453 & VMRn =303) | Total% | |
| Allergic rhinitis (AR)(N= 1390) | 57% | 93% | 68.8% |
| Vasomotor rhinitis(VMR)(N= 916) | 49% | 89% | 62% |
| Total N = 2306 | 54% | 92% | 66.1% |
| Type of general pathology | Percentage (%) of post-operative epistaxis (E) and recurrence of nasal obstruction (RNO) at each procedure in relation to patients' general health status | |||
| SMD (N=1550)(HTNn= 47 & DMn =81) | PIT (N=756)(HTNn= 13& DMn =37) | |||
| E | RNO | E | RNO | |
| Systemic hypertension (N= 67) | 27% | 39% | 91% | 13% |
| Diabetes mellitus(N= 122) | 19% | 87% | 73% | 17% |
| The items | The expenses for different inferior turbine surgery techniques in Libyan dinars (mean± standard error of mean (s. e. m)) | |
| SMD | PIT | |
| Drugs | 108±4.7 | 324±5.3 |
|---|---|---|
| Nasal packing | 46±11.5 | 100±0.2 |
| Patients word stay | 378±3.9 | 897±0.7 |
| Post-operative patient follow-up | 105±4.3 | 231±6.3 |
| The total in Libyan dinars | 637±5.7 | 1552±7.1 |
| The total in American dollars | 126±2.9 | 558±3.7 |
| Outcomes | Percentage of outcomes with septoplasty N=924 | Percentage of outcomes without septoplasty N=1382 | ||
| One point SMD n= 554 | One-third PIT n= 370 | Two point SMD n=999 | Two-thirds PIT n=383 | |
| Atrophic changes | 0 | 2% | 31% | 47% |
|---|---|---|---|---|
| Persistent nasal obstruction | 0 | 0 | 12% | 9% |
Discussion
The inferior concha surgery is commonly performed therefore it always needs to improve its outcomes. Although during last two centuries there are many published clinical studies which tried to present new techniques that may had been proved with better outcomes of this surgery but still as concluded at other many clinical trials and observations that it may become very difficult to decide which technique is most suitable modality for the selected candidate. It was found that there are many factors, which may be determine difficulties regarding the selection of most proper manner of inferior conchae surgery 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40. However most of the recent studies tried to resolve these difficult situations but from the surgical side it was noted that in spite of following of these studies recommendations, unpredicted post-operative outcomes still appearing. Thus this type of surgery can be classified as one of the dilemmas at rhinology.
Regarding the selection of the patient who should be considered as most suitable candidate for inferior turbinate surgery, generally speaking the inferior conchae surgery can be elective and non-elective i.e. when this pattern of surgery is decided to be performed for the management of persistent mechanical nasal obstruction at this case it will be classified as elective surgery 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20. On the other hand, the inferior turbinatectomy can be conducted non-electively as a part of wide resection of sino-nasal neoplastic lesions 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40. Our discussion is mainly highlight the elective category of this surgery. Basically there are five major criteria according to which the patient might be indicated for inferior concha surgery:
The patient has chronic nasal obstruction related presentations this can be as partial or complete inability to breathe through the nose, frequent or persistent opened mouth for mouth breathing, olfaction function impairment, sleep related breathing disorders, and recurrent sore throat, pharyngitis, as well as oral ulcers due to persistent mouth breathing.
The patient received sufficient medical therapy in form of local steroids, local nasal douching, systemic steroids, and systemic anti-histamines for enough time which is 3-6 months but the patient did not show any significant clinical improvement.
The patient proved locally that has significant (HIC) which occupies more than one-third of nasal cavity.
The HIC grossly appears as enlarged turbinate with thick, pale, grayish-white, and non-shiny covering mucosa.
The significant nasal obstruction due to HIC, must be elucidated objectively by positive rhino-metric evaluation, and\ or positive Cottle's sign, and\ or positive impairment of olfactory function.
Hence, the patient was selected as indicated candidate for inferior turbinate surgery; the next step will be the selection of most proper technique for that particular patient. there are two modalities of inferior turbinate surgical techniques namely; a) PIT which can be done by lateral resection of maximum up to one-third of HIC either by using curved scissors, or shaver, or radio-frequency ablation, or co-ablation 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41. b) SMD, this technique is considered as old fashion for inferior turbinate surgery. It is performed by creation of electrical cauterization at multiple points (2-5 points) through sub-mucosal layer of HIC. This technique acts mainly by cauterization of sub-mucosal venous sinusoids among HIC with active sensitization inflammatory process due to allergic rhinitis, vasomotor rhinitis, or rhinitis medica-mentosa. Thus the sub-mucosal fibrosis will be induced subsequently as a reaction to venous sinusoids cauterization and this will result in the shrinkage of inferior turbinate bulk. However, the submucosal diathermy technique was proved very effective and simple technique but still it is of no benefits among those patients with HIC due to increase in bulk of concha bone rather than soft tissue 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20.
We noted throughout our long-term experience, which extend for more than fifteen years that the following of the recommendations that usually came out from several old as well as recent studies regarding inferior conchae surgeries did not sufficiently give the suggested results as those studies concluded. For this reason, we tried through this proposed serial study to predict the factors that may had been thought to be significant factors affecting outcomes of this surgery. Moreover, these studied factors can be discussed as: a) Patient's age, the elderly patients showed higher incidence of post-operative epistaxis and the atrophic rhinitis as compared to the younger people. In the same manner, the incidence of post-operative epistaxis as well as atrophic rhinitis significantly increased by interfering with PIT as compared to SMD. This can be explained by basic-physiological fact, that vascular related aging process among elderly patients constitutes the major predisposing factor for the impairment of local homeostasis control after the surgery and the delay of proper healing process at the site of surgery. Also, the significant decrease in the number of venous sinusoids and mucosal glandular acini at sub-mucosal layer of the concha among elderly patient. 1, 2, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45. Thus PIT might not be considered as most suitable selection for inferior conchae surgery among old ages. b) Patient related habitual and environmental factors, there was significant increased the incidence of post-operative recurrence of HIC by smoking and chronic exposure to certain allergens as pollens, animal epithelial, house dust mites, and chemical irritants as compared to the non-smokers and those patients who are not frequently exposed to environmental irritants. c) Patient's local health status, as can be elucidated from this serial study that the local nasal pathological status of the patient might affect significantly the decision regarding the selection of most proper technique of inferior concha surgery. i.e. those patients who presented as cases of allergic rhinitis and vasomotor rhinitis got significant long standing improvement regarding the patency of nose after PIT as compared to SMD. This might be due to the sufficient amount of tissue which resected by PIT. On the other hand, the basic idea behind the conduction of SMD is to reduce the number of venous sinusoids and to stimulate the diffuse fibrosis at the level of sub-mucosal layer of inferior turbinate. These effects had been proved to be not sufficient to fulfill the adequate maintenance of optimum size of inferior turbinate because still there is risk of re-proliferation of the venous sinusoids and recurrence of hypertrophy of inferior turbinate. Thus, the most suitable techniques for inferior turbinate surgery among patients with allergic rhinitis or vasomotor rhinitis is PIT 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31. d) Patient's systemic health status, this presenting study demonstrated that the risk of epistaxis is increased after PIT among hypertensive patients as well as diabetic patients; this can be explained by extensive local tissue injury due to PIT as compared to other less invasive techniques. in accordance, the SMD results in increased risk of recurrence of nasal obstruction among patients with diabetes mellitus as compared to PIT. This can be reasoned to that, the patients with diabetes mellitus are more prone for local atrophic changes and diffuse fibrosis as compared to non-diabetic patients. This is due to high incidence of local diabetic angiopathic changes. In addition, the higher incidence of vasomotor rhinitis among diabetic patients as compared to non-diabetic patients, this will increase the risk of recurrence of mechanical nasal obstruction due to inferior turbinate hypertrophy. Accordingly, we can recommend that the PIT is not the suitable technique for hypertensive and diabetic patients; also, SMD is not the curable procedure for patient with diabetes mellitus 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29.
In same manner, there is another important factor, which may play an important role in the rooting of these difficulties of this surgery namely the socio-economic factor. As it was illustrated from this study and via the rough evaluation of different economic aspects for each performed technique, including the expense of used drugs, nasal packing, patient word stay, and post-operative patient follow-up it was found that PIT had higher prices as compared to SMD. The PIT is described as more invasive technique which consume longer operative duration thus the amount of utilized anesthesia drugs will be more. in addition to certain specific drugs which might be needed to be administrated as tranxiemic acid for purpose of epistaxis control which will be more among PIT 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45. In accordance, patients after PIT need to be cared more as compared to other technique this will result in the prolongation of patient's post-operative stay at word. In addition, the patients after PIT needs repetitive follow-up sessions. This is because of high tendency for recurrent local dryness and crusts formation during first 4-6 weeks post-operatively, which may predispose to infective rhinitis that leads to healing by scaring and synaechia formation. However the PIT is representing a very effective procedure for the surgical management of persistent mechanical nasal obstruction due to HIT but still it is considered as expensive procedures as compared to SMD 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 45.
From the other view, we tried at our serial to postulate whether the concomitant septoplasty has any role regarding improvement of outcomes of inferior concha surgery. Indeed, we found that the septoplasty even for mild deviated nasal septum as bothersome procedure with inferior concha surgery might improve significantly the outcomes of this surgery. This can be reasoned by reducing the points of cauterization among SMD cases and limitation of the tissue resection among PIT cases. Thus, the risk of post-operative functional nasal obstruction due to atrophic rhinitis is significantly decreased 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45.
Finally, we can conclude to that really the inferior concha surgery is considered as one of difficult dilemmas at rhinology and because it is widely conducted surgery thus always, it needs frequent research to resolve all possible associated problems and issues 45. The cornerstone of this dilemma is how to avoid the adverse outcomes of inferior concha surgery45. As it can be noted from the results of this serial study, the results were confirming and approving the conclusion of our previously conducted study on 201545 We tried through this serial study to extend our previous study just by increasing the number of cases and expand the period of follow up for the operated patients45.
Although this study was not so well-controlled, but it is long-standing, and of adequate number of cases, but as previous study. Therefore, as other suggested recommendation, the further clinical studies are advised to be committed to confirm these concepts which obtained from this presenting study and in the same time the new aims may be suggested to be illustrated to find proper answer for these big titled questions.
References
- 1.Takeuchi H, Jawad M, Eccles R. (2000) Changes in unilateral nasal airflow in patients with seasonal allergic rhinitis measured in and out of season. , Auris Nasus Larynx 27(2), 141-5.
- 2.Fradis M, Malatskey S, Magamsa I, Golz A. (2002) Effect of submucosal diathermy in chronic nasal obstruction due to turbinate enlargement. , Am J Otolaryngol 23(6), 332-6.
- 3.Li P. (2001) The effect of submucosal diathermy to the inferior turbinates on nasal airway resistance. 15(8), 354-5.
- 4.Farmer S E, Quine S M, Eccles R. (2009) Efficacy of inferior turbinate coblation for treatment of nasal obstruction. , J Laryngol Otol 123(3), 309-14.
- 5.Ikeda K, Oshima T, Suzuki M, Suzuki H, Shimomura A. (2006) Functional inferior turbinosurgery (FITS) for the treatment of resistant chronic rhinitis. , Acta Otolaryngol 126(7), 739-45.
- 6.Gindros G, Kantas I, Balatsouras D G, Kandiloros D, Manthos A K et al. (2009) Mucosal changes in chronic hypertrophic rhinitis after surgical turbinate reduction. , Eur Arch Otorhinolaryngol 266(9), 1409-16.
- 7.Bäck L J, Hytönen M L, Malmberg H O, Ylikoski J S. (2002) Submucosal bipolar radiofrequency thermal ablation of inferior turbinates: a long-term follow-up with subjective and objective assessment. , Laryngoscope 112(10), 1806-12.
- 8.Chen Y L, Tan C T, Huang H M. (2008) Long-term efficacy of microdebrider-assisted inferior turbinoplasty with lateralization for hypertrophic inferior turbinates in patients with perennial allergic rhinitis. , Laryngoscope 118(7), 1270-4.
- 9.Chen Y L, Liu C M, Huang H M. (2007) Comparison of microdebrider-assisted inferior turbinoplasty and submucosal resection for children with hypertrophic inferior turbinates. , Int J Pediatr Otorhinolaryngol 71(6), 921-7.
- 10.Mori S, Fujieda S, Yamada T, Kimura Y, Takahashi N et al. (2002) Long-term effect of submucous turbinectomy in patients with perennial allergic rhinitis. , Laryngoscope 112(5), 865-9.
- 11.Ogawa T, Takeno S, Ishino T, Hirakawa K. (2007) Submucous turbinectomy combined with posterior nasal neurectomy in the management of severe allergic rhinitis: clinical outcomes and local cytokine changes. Auris Nasus Larynx. 34(3), 319-26.
- 12.Schmidt J, Zalewski P, Olszewski J, Olszewska-Ziaber A. (2001) Histopathological verification of clinical indications to partial inferior turbinectomy. , Rhinology 39(3), 147-50.
- 13.Ishida H, Yoshida T, Hasegawa T, Mohri M, Amatsu M. (2003) Submucous electrocautery following submucous resection of turbinate bone--a rationale of surgical treatment for allergic rhinitis. Auris Nasus Larynx. 30(2), 147-52.
- 14.Chhabra N, Houser S M. (2011) The surgical management of allergic rhinitis. , Otolaryngol Clin North Am 44(3), 779-95.
- 15.Vijay Kumar K, Kumar S, Garg S. (2014) A comparative study of radiofrequency assisted versus microdebrider assisted turbinoplasty in cases of inferior turbinate hypertrophy. , Indian J Otolaryngol Head Neck Surg 66(1), 35-9.
- 16.Cavaliere M, Mottola G, Iemma M. (2005) Comparison of the effectiveness and safety of radiofrequency turbinoplasty and traditional surgical technique in treatment of inferior turbinate hypertrophy. Otolaryngol Head Neck Surg. 133(6), 972-8.
- 17.Rhee C S, Kim D Y, Won T B, Lee H J, Park S W et al. (2001) Changes of nasal function after temperature-controlled radiofrequency tissue volume reduction for the turbinate. , Laryngoscope 111(1), 153-8.
- 18.Cassano M, Granieri C, Del Giudice AM, Mora F, Fiocca-Matthews E et al. (2010) Restoration of nasal cytology after endoscopic turbinoplasty versus laser-assisted turbinoplasty. , Am J Rhinol Allergy 24(4), 310-4.
- 19.Lorenz K J, Maier H. (2013) Microdebrider-assisted inferior turbinoplasty. Minimally invasive technique for the treatment of nasal airway obstruction caused by enlarged turbinates. , HNO 61(3), 240-9.
- 20.Yanez C, Mora N. (2008) Inferior turbinate debriding technique: ten-year results. Otolaryngol Head Neck Surg. 138, 170-5.
- 21.Sacks R, Thornton M A, Boustred R N. (2008) Modified endoscopic turbinoplasty - long term results compared to submucosal electrocautery and submucosal powered turbinoplasty. Presented at the American Rhinologic Society.
- 22.Passali D, Passali F M, Damiani V, Passali G C, Bellussi L. (2003) Treatment of inferior turbinate hypertrophy: a randomized clinical trial. Ann Otol Rhinol Laryngol. 112, 683-688.
- 23.VWS Lai, Corey J P. (1993) The objective assessment of nasal patency. , Ear Nose Throat J 72, 395-400.
- 24.Seeger J, Zenev E, Gundlach P. (2001) Bipolar radiofrequency-induced thermotherapy of turbinate hypertrophy: pilot study and 20 months follow-up. , Laryngoscope 113, 130-5.
- 25.Camelo-Nunes I C, Solé D. (2010) Allergic rhinitis: indicators of quality of life. , J Bras Pneumol 36(1), 124-33.
- 26.Stewart M G, Witsell D L, Smith T L, Weaver E M, Yueh B et al. (2004) Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg. 130(2), 157-63.
- 27.Stewart M G, Smith T L, Weaver E M, Witsell D L, Yueh B et al. (2004) Outcomes after nasal septoplasty: results from the Nasal Obstruction Septoplasty Effectiveness (NOSE) study. Otolaryngol Head Neck Surg. 130(3), 283-90.
- 28.Cavaliere M, Mottola G, Iemma M. (2005) Comparison of the effectiveness and safety of radiofrequency turbinoplasty and traditional surgical technique in treatment of inferior turbinate hypertrophy. Otolaryngol Head Neck Surg. 133(6), 972-8.
- 29.Bhandarkar N D, Smith T L. (2010) Outcomes of surgery for inferior turbinate hypertrophy. Curr Opin Otolaryngol Head Neck Surg. 18(1), 49-53.
- 30.Leong S C, Eccles R. (2010) Inferior turbinate surgery and nasal airflow: evidence-based management. Curr Opin Otolaryngol Head Neck Surg. 18(1), 54-9.
- 31.Hol M K, Huizing E H. (2000) Treatment of inferior turbinate pathology: a review and critical evaluation of the different techniques. , Rhinology 38(4), 157-66.
- 32.Hanif J, Jawad S S, Eccles R. (2000) The nasal cycle in health and disease. Clin Otolaryngol Allied Sci. 25(6), 461-7.
- 33.Farmer S E, Eccles R. (2006) Chronic inferior turbinate enlargement and the implications for surgical intervention.Rhinology. 44(4), 234-8.
- 34.Bhandarkar N D, Smith T L. (2010) Outcomes of surgery for inferior turbinate hypertrophy. Curr Opin Otolaryngol Head Neck Surg. 18(1), 49-53.
- 35.Ozcan K M, Gedikli Y, Ozcan I, Pasaoglu L, Dere H. (2008) Microdebrider for reduction of inferior turbinate: evaluation of effectiveness by computed tomography. , J Otolaryngol Head Neck Surg 37(4), 463-8.
- 36.Chhabra N, Houser S M. (2009) The diagnosis and management of empty nose syndrome. , Otolaryngol Clin North Am 42(2), 311-30.
- 37.Batra P S, Seiden A M, Smith T L. (2009) Surgical management of adult inferior turbinate hypertrophy: a systematic review of the evidence. , Laryngoscope 119(9), 1819-27.
- 38.Tanna N, Im D D, Azhar H, Roostaeian J, Lesavoy M A et al. (2014) Inferior turbinoplasty during cosmetic rhinoplasty: techniques and trends. Ann Plast Surg. 72(1), 5-8.
- 39.Schumacher M J. (2004) Nasal dyspnea: the place of rhinomanometry in its objective assessment. , Am J Rhinol 18(1), 41-6.
- 40.Eccles R, Jawad M S, Jawad S S, Angello J T, Druce H M. (2005) Efficacy and safety of single and multiple doses of pseudoephedrine in the treatment of nasal congestion associated with common cold. , Am J Rhinol 19(1), 25-31.
- 41.Garzaro M, Pezzoli M, Landolfo V, Defilippi S, Giordano C et al. (2011) Radiofrequency Inferior Turbinate Reduction: Long-Term Olfactory and Functional Outcomes. Otolaryngol Head Neck Surg.
- 42.Tanna N, Lesavoy M A, Abou-Sayed H A, Gruber R P. (2013) . , Septoturbinotomy. Aesthet Surg 33(8), 1199-205.
- 43.Gupta A, Mercurio E, Bielamowicz S. (2001) Endoscopic inferior turbinate reduction: an outcomes analysis. Laryngoscope. 2001; 111(11 Pt 1, 1957-9.
