Comparing Uterine Electromyography & Tocodynamometer to Intrauterine Pressure Catheter for Monitoring Labor
Abstract
Objective
The tocodynamometer (TOCO) has poor sensitivity and specificity in monitoring uterine contractions, especially in obese patients. The intrauterine pressure catheter (IUPC) can be used to monitor adequacy of contractions, but only after amniotomy. Transabdominal uterine electromyography (EMG) and the TOCO were compared to the gold standard IUPC for monitoring uterine contractions.
Methods
Forty term pregnant women in labor with ruptured membranes were consented for this study. The root mean square (RMS) plot from EMG signals was compared to IUPC and TOCO recordings for 20 to 40 minutes. A comparison between the total contraction number, frequency, and the difference in contraction peak time was made using Student-t test or ANOVA (P<0.05 was significant).
Results
There was no significant difference in the contraction number and frequency when comparing the RMS, TOCO, and IUPC. The paper tracings had a greater standard deviation (8.57) than the digitally saved data (3.93). The mean peak time difference between TOCO and IUPC was 0.74 seconds (P=0.78; SD 5.2). For RMS vs. IUPC peaks, the mean peak difference between was 0.13 seconds (P=0.95; SD 3.93).
Conclusions
Uterine electrical activity measured with transabdominal uterine EMG may be used to monitor labor in patients as an alternative to the TOCO and the IUPC.
Author Contributions
Academic Editor: Baris Baykal, Assisted Reproductive Techniques Centre, Department of Obstetrics and Gynecology, School of Medicine, Gulhane Military Medical Academ
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Sangeeta Jain, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Women in labor are traditionally monitored with the tocodynamometer (TOCO), which is based on the pressure force produced by the contorting abdomen during uterine contractions. The contractions are measured by a pressure transducer placed on the patient’s abdomen. For this instrument, a belt is wrapped around the patient’s abdomen, which can be very uncomfortable and constraining 1. The device has also been found to be inaccurate, its measurements subjective and dependent upon how tight the belt is applied. The intrauterine pressure catheter (IUPC), often considered as the reference (gold) standard, can be utilized only after amniotomy (ruptured membranes). There is a learning curve associated with the technique of correctly placing an IUPC. It has been reported that as many as 30% may be placed “extra membranous,” leading to the increased risk of artefactual waveforms, placental perforation, abruption, and uterine rupture 2.
Uterine smooth muscle contraction is an electrochemical process 3, 4. Transabdominal uterine electromyography (EMG) measures the action potentials of the uterine smooth muscles in the form of electrical bursts (spikes) with the help of surface electrodes (Figure 1). The signal function is based upon the fact that the myometrial electrical activity is responsible for uterine smooth muscle contraction and relaxation, similar to the electrocardiogram, which measures the cardiac smooth muscle electrical depolarization and its passage in the heart. A series of spikes together generate a contraction. Transabdominal uterine EMG has been studied at varying gestational ages with increased electrical activity seen both in term and preterm labor 5. It may identify patients who deliver within 24 hours of measurement 6. Others show that the signals generated in normal, preterm, and arrested labor appear significantly different, allowing clinical interpretation of the labor progress 7, 8, 9. Transabdominal uterine EMG has higher negative (NPV: 90) and positive predictive values (PPV: 82) to identify patients in preterm labor compared to parameters like preterm labor symptoms, cervical length, fetal fibronectin, and salivary estriol (NPV: 86 to 89; PPV: 21 to 43) 10. Since uterine EMG has been shown to positively correlate with uterine activity and progression of labor, this study was conducted to see whether it may be used as a noninvasive alternative to the TOCO and the IUPC.
Figure 1.Patient with the uterine electromyography electrodes, the tocodynamometer transducer and the fetal heart rate Doppler applied to the abdomen.
Objectives
To compare the performance of the uterine EMG and TOCO to the IUPC in detection of uterine contractions in term laboring patients.
To evaluate the agreement of the uterine contraction peak times in uterine EMG, the TOCO, and the IUPC in term laboring patients.
Materials and Methods
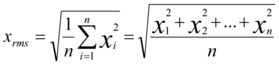
After obtaining approval from the Institutional Review Board (IRB), pregnant women at term gestation, in labor, with ruptured membranes and an IUPC in place, were consented for the study at the University of Texas Medical Branch at Galveston. Those with multifetal pregnancy, fetal anomaly, vaginal bleeding, or a history of cervical surgery were excluded. The instrument connections were as shown in Figure 2. The electrodes were self-adhesive Ag 2Cl models, each approximately 2cm2 in area (Quinton, Bothell, Washington). Grounding was accomplished by placing a wire laterally on the patient’s hip. The acquisition/storage system was a custom “Surecall” system provided by Reproductive Research Technologies, Houston, TX. Filtering for 0.2 to 2.0 Hz band-pass, signals were sampled at 100 Hz. Signals were then digitally filtered to band-pass only the uterine-specific frequencies of 0.3 to 1.0 Hz 11. The purpose of digital filtering (used Lab View) was to remove any signal noise outside the frequency envelope of interest which was the uterine –specific frequency in this case. The root mean square (RMS) transform was thereafter applied to the EMG signals by using a running window with a length of 3000 data points through the EMG recordings. This value was determined by evaluating our initial training data and trying to produce an RMS signal that closely matched the IUPC in shape and smoothness. At these threshold values, the best RMS signal recording was obtained appearing similar to the IUPC on the visual tracing. The RMS of a collection of n values (in our case, 3000 data points) is:
where x is the magnitude of a single EMG data
sample (the SureCALL records 100 each second) and n is the number of samples set in the RMS Buffer. The x labeled RMS is the RMS magnitude recorded for each window of EMG samples. This technique was applied to all data in EMG records to identify and plot contraction events and generate a visual tracing which can be compared to that of the TOCO and IUPC.
The recordings from the subjects were performed for 20 to 40 minutes. The contraction plot recordings printed on paper produced by the traditional TOCO and IUPC were compared to the digitally-time-stamped traces routed through the SureCall EMG System.
Figure 2.Configuration of the instruments applied to the subject for simultaneous recording and comparison.
Analysis
A contraction measured as RMS by the uterine EMG is considered to be present if the signal inflection is greater than 30 seconds in duration and the amplitude of the signal is ≥1/9 of the amplitude from the greatest contraction peak to the lowest baseline in the trace (referred to as an “arbitrary unit”).
A contraction event was considered to be measured by RMS, IUPC, or TOCO if there was an observed increase in the contraction trace value from a local baseline, immediately followed by a peak in the contraction trace value, which was, in turn, immediately followed by a subsequent decrease in the contraction trace value to a local baseline. Correspondence between 2 devices’ contraction plots was defined when an event occurred simultaneously in both devices’ signals, with a 50% temporal overlap. A contraction plot made by one device was not considered to be a corresponding contraction if it was more than twice the duration of the other device’s potential corresponding contraction.
A mean peak-point difference was found for each subject, and the peak points of the contraction plots from the 3 devices were compared since early and late decelerations of the fetal heart tones are defined based on their location with respect to the contractions seen with the IUPC.
No sample size/power calculations were done for this study as this was an exploratory comparative study. Typically, a group size of 20-40 subjects is generally enough. The total number of contractions and the differences in their peak time values were evaluated using Statistical analysis was performed using Friedman Repeated Measures Analysis of Variance on Ranks followed by multiple comparison Student-Newman-Keuls Method. Shapiro-Wilk test was performed for normality. A p-value less than 0.05 was considered statistically significant. The positive percent agreement (PPA), negative percent agreement (NPA), and overall percent agreement (OPA) between the devices was calculated using a bootstrap method. The IUPC, RMS, and TOCO peaks were also analyzed using the mixed model analysis in order to account for the within-patient contraction number variability.
Results
A total of 40 pregnant women were enrolled in the study. Maternal age, BMI, presence or absence of pitocin augmentation, and the total number of contraction peaks observed from each device in each subject are shown for both printed and digitally-saved/time-stamped tracings in Table 1. There was no significant difference seen in any of these parameters.
Table 1. There was no significant difference seen in any of these parameters. There was good visual correspondence between the 3 contraction plotting devices shown in.| Patient (digital | Maternal Age | BMI | Pitocin Augmentation | Total IUPC | Total RMS | Total TOCO |
| traces) | (Years) | Contractions(Frequency) | Contractions(Frequency) | Contractions(Frequency) | ||
| 1 | 35 | 29 | Yes | 7 | 9 | 9 |
| 2 | 30 | 28.7 | No | 15 | 14 | 26 |
| 3 | 20 | 31.6 | Yes | 10 | 10 | 10 |
| 4 | 24 | 27 | Yes | 10 | 10 | 9 |
| 5 | 27 | 38.8 | Yes | 6 | 6 | 6 |
| 6 | 29 | 33 | No | 11 | 13 | 11 |
| 7 | 24 | 25.7 | No | 12 | 9 | 11 |
| 8 | 21 | 31.9 | No | 14 | 14 | 14 |
| 9 | 24 | 39.2 | Yes | 14 | 12 | 14 |
| 10 | 21 | 30.1 | Yes | 12 | 12 | 11 |
| 11 | 20 | 39.5 | No | 13 | 13 | 13 |
| 12 | 18 | 39.9 | Yes | 12 | 13 | 12 |
| 13 | 24 | 36.9 | No | 9 | 11 | 8 |
| 14 | 20 | 33.1 | Yes | 12 | 12 | 12 |
| 15 | 18 | 37 | No | 16 | 16 | 14 |
| 16 | 24 | 37.8 | Yes | 8 | to | 8 |
| 17 | 18 | 25.2 | Yes | 11 | 11 | 11 |
| 18 | 18 | 30.5 | Yes | 13 | 13 | 13 |
| 19 | 20 | 26.6 | Yes | 12 | 10 | 12 |
| 20 | 18 | 23.6 | Yes | 19 | 18 | 15 |
| 21 | 26 | 332 | Yes | 10 | 11 | 10 |
| 22 | 30 | 302 | Yes | 16 | 16 | 16 |
| 23 | 27 | 34.8 | No | 13 | 13 | 13 |
| 24 | 27 | 363 | Yes | 16 | 16 | 16 |
| 25 | 18 | 35.1 | No | 19 | 19 | 19 |
| 26 | 31 | 33.1 | No | 5 | 5 | 5 |
| 27 | 29 | 29 | Yes | 12 | 12 | 13 |
| 28 | 27 | 23.6 | No | 14 | 14 | 14 |
| 29 | 28 | 31.8 | Yes | 10 | 10 | 11 |
| 30 | 19 | 42.2 | No | 11 | 11 | 11 |
| 31 | 25 | 29.2 | Yes | 13 | 13 | 13 |
| 32 | 29 | 32.1 | Yes | 10 | 10 | 10 |
| 33 | 29 | 26.9 | Yes | 15 | 15 | 15 |
| 34 | 23 | 26.2 | Yes | 18 | 18 | 18 |
| 35 | 25 | 34.6 | Yes | 13 | 13 | 13 |
| 36 | 20 | 35.5 | Yes | 13 | 13 | 13 |
| 37 | 17 | 32.6 | Yes | 9 | 9 | 9 |
| 38 | 27 | 31.4 | No | 13 | 3 | 13 |
| 39 | 21 | 31.6 | Yes | 10 | 10 | 9 |
| 40 | 19 | 36.2 | Yes | 13 | 13 | 13 |
| Total(Mean±SD) | 23.28 | 32.27 | N/A | 489 | 490 | 493 |
There was good visual correspondence between the 3 contraction plotting devices shown in Figure 3. The fetal heart rate tracing could potentially be evaluated in a similar manner as with the TOCO and IUPC. In 3 patients, there was some additional uterine smooth muscle activity seen on the RMS not seen in the IUPC or TOCO. This was inferred to be firing of signals from a group of smooth muscles not significant enough to cause a meaningful contraction (CTX). These were not associated with any change in fetal heart rate pattern. With regards to both the CTX number and frequencies, there was no statistical differences between the three different modalities (Figure 4). The difference in frequency of CTXs between RMS and IUPC was 0.42±0.07 compared to TOCO and IUPC which was 0.44±0.14. As expected, the digitally saved time-stamped data showed greater agreement percentage (98.5%–100%) than the printed paper tracings (91.5%–94%).
Figure 3.Simultaneous recording and comparison of the signals (from top to bottom): the raw EMG signal, the IUPC recording. The external TOCO recording and the RMS signal from a single subject. Note the exceptional correspondence between RMS-plotted contractions and the IUPC-plotted contractions.
Figure 4.No differences were noted in contraction numbers among the TOCO, RMS and IUPC groups in printed time-stamped tracings (Panel A; P=0.779) and digitally-saved/time-stamped tracings (B; P=0.327). Same observations were noted in frequency of contractions in printed time-stamped tracings (Panel C; P=0.327) and digitally-saved/time-stamped tracings (D; P=0.779). Analysis was performed using Friedman Repeated Measures Analysis of Variance on Ranks followed by multiple comparison Student-Newman-Keuls Method. Shapiro-Wilk test was performed for normality. A p-value less than 0.05 was considered statistically significant.
Discussion
Literature review showed Ramondt et al have described EMG and IUPC from chronically instrumented ovariectomised ewe to develop a program for computer-aided analysis of the electrical and mechanical activity of the myometrium 11. Our study shows its application in pregnant human subjects. In fact, this is the first study comparing transabdominal uterine EMG to the TOCO and IUPC in term laboring patients with spontaneous or artificially ruptured membranes.
Jezewski et al compared EMG to TOCO in term pregnant women not in labor and found high agreement and consistency in the number of CTXs between the two 13. Our study further supports this by comparing with the IUPC, the gold standard. In fact, when we look at each subject recordings, the RMS recordings correlated well with the IUPC even in the subjects where the TOCO did not do so well. In some instances, the RMS showed evidence of some smooth muscle electrical activity which was not strong enough to make a contraction in the IUPC signal or the TOCO, but unlike the TOCO, the RMS never missed a contraction signal picked up by the IUPC. This shows the high sensitivity of the RMS to uterine smooth muscle electrical activity. Also, there was no significant difference in the recording from the 3 devices with or without pitocin augmentation.
Subjects with varying BMIs ranging from 26 to 42.2 were included in the study with no difference in the EMG recordings. Euliano et al studied the pattern of uterine electrical activity in 7 obese pregnant women who later underwent IUPC placement and found that the TOCO had been unreliable in picking uterine contractions in obese women 14. The electrohysterogram-derived contraction pattern in that study correlated better with the IUPC than the TOCO. Our study agrees with this that adipose tissue does not interfere with the transmission of uterine smooth muscle electrical signals as it does with the TOCO signal. Further studies are being done to compare uterine EMG in various classes of obesity.
When comparing the contraction-plotting characteristics of these clinical devices, it is useful to know how well the devices “match-up” with regard to the frequency of the contractions since it is routinely used to assess labor. The lower PPA and NPA values in the printed paper tracing clearly showed the digitally saved time-stamped data to be far superior.
The high correspondence between contraction plots and the absence of differences in contraction frequency rates indicates that EMG, rather than the TOCO, can be used to assess contraction frequency. The absence of differences in contraction peak times suggests that there may not be clinical differences in the interpretation of fetal heart rate tracing (early and late decelerations) using EMG rather than the IUPC. The sensitivity and specificity of uterine EMG have been consistently found to be around 90% in predictive studies of labor and delivery 12, giving an additional advantage of using uterine EMG rather than TOCO, which seems to have no predictive value in this regard 15. The EMG could be used to study other parameters such as relative amplitudes within a trace, shape parameters of the contractions and frequency domain analysis. We would like to start evaluating some different parameters that show potential. In present study, the parameters that were of interest to the US Food & Drug Administration (FDA) were shown.
This study data was submitted and received US Food & Drug Administration (FDA) approval for the EMG machine to be used in term pregnant women. One of the limitations of this study is that it is an explorative study comparing different modalities for detecting uterine contractions, hence our results should not be used for supporting uterine EMG as a replacement for the IUPC. Future prospective randomized control study with enough power are needed to address the clinical outcomes between both modalities. The RMS signal cannot be used to calculate Montevideo’s units (MVUs) as we do in case of IUPC. MVUs are calculated by multiplying the number of CTXs in 10 minutes to the amplitude of the CTX. This study does not compare the amplitude of the contractions recorded by the IUPC to the RMS to look for correspondence. However, previous work has already indicated a strong correspondence of uterine EMG “energy” with certain IUP measures 15. It certainly is a better alternative to the TOCO when each case is studied individually.
The study shows that transabdominal uterine electrical recordings, along with the RMS transform, can be used to generate contraction tracings similar in appearance to TOCO and IUPC recordings and may be used to assess term labor. Contraction events in pregnant patients can be monitored and evaluated non-invasively by the uterine EMG, without the need for the discomfort of the TOCO or the additional cost and invasiveness of the IUPC. The uterine EMG device has now FDA approval for use to monitor term patients in labor instead of the traditional TOCO. Further powered studies are needed to draw definite conclusions and its use for diagnosing normal and abnormal uterine function, both in clinical and research settings.
Glossary
IUPC: intrauterine pressure catheter
EMG: electromyography
TOCO: tocodynamometer
RMS: root mean square
NPV: negative predictive value
PPV: positive predictive value
IRB: Institutional review board
PPA: positive percent agreement
NPA: negative percent agreement
OPA: overall percent agreement
Acknowledgements
We would like to thank Dr. R. Fink, Dr. Garfield and Reproductive Research Technologies for their support in providing the SureCall EMG monitor and accessories.
References
- 1.Hodnett E. (1982) Patient control during labor. Effects of two types of fetal monitors. , JOGN Nurs 11, 94-9.
- 2.Lind B K. (1998) The frequency of extra membranous placement of intrauterine pressure catheters. Prim Care Update Ob Gyn. 5, 185.
- 3.Marshall J M. (1962) Regulation of activity in uterine smooth muscle. Physiol Rev,42(Suppl.5):. 213-7.
- 4.Kuriyama H. (1961) recent studies of the electrophysiology of the uterus. Study group no.9. Progesterone & Defense mechanism of pregnancy. London:Churchill 51-71.
- 5.Buhimschi C, Boyle M B, Garfield R E. (1997) Electrical activity of the human uterus during pregnancy as recorded from the abdominal surface. , Obstet Gynecol 90, 102-11.
- 6.Garfield R E, Maner W L, MacKay L B, Schlembach D, Saade G R. (2005) Comparing uterine electromyography activity of antepartum patients versus term labor patients. , Am J Obstet Gynecol 193, 23-9.
- 7.Most O, Langer O, Kerner R, David G B, Calderon I. (2008) Can myometrial electrical activity identify patients in preterm labor?. , Am J Obstet Gynecol,199: 378-1.
- 8.Euliano T Y, Marossero D, Nguyen M T. (2009) Spatiotemporal electrohysterography patterns in normal and arrested labor. , Am J Obstet Gynecol 200, 54-1.
- 9.Diab M O, Marque C, Khalil M. (2009) An unsupervised classification method of uterine electromyography signals: Classification for detection of preterm deliveries. , J Obstet Gynaecol 35, 9-19.
- 10.Garfield R E, Maner W L. (2007) Physiology and electrical activity of uterine contractions. , Sem Cell Dev Biol 18, 289-95.
- 11.Ramondt J, C Van Kooten, Verhoeff A, HCS Wallenburg. (1986) Computer analysis of mechanical and electrical uterine activity. , Med & Biol. Eng & Comput 24, 351-355.
- 12.Maner W L, Garfield R E, Maul H, Olson G, Saade G. (2003) Predicting term and preterm delivery with transabdominal uterine electromyography. , Obstet Gynecol 101, 1254-60.
- 13.Jezewski J, Horoba K, Matonia A, Wrobel J. (2005) Quantitative analysis of contraction patterns in electrical activity signal of pregnant uterus as an alternative to mechanical approach. , Physiol. Meas 26, 753-767.
Cited by (4)
- 1.Wang Hui, Wu Wenjie, Talcott Michael, McKinstry Robert C., Woodard Pamela K., et al, 2020, Accuracy of electromyometrial imaging of uterine contractions in clinical environment, Computers in Biology and Medicine, 116(), 103543, 10.1016/j.compbiomed.2019.103543
- 2.Saleem Saqib, Saeed Ahmed, Usman Shabnam, Ferzund Javed, Arshad Jahangir, et al, 2020, Granger causal analysis of electrohysterographic and tocographic recordings for classification of term vs. preterm births, Biocybernetics and Biomedical Engineering, 40(1), 454, 10.1016/j.bbe.2020.01.007
- 3.Peng Jin, Hao Dongmei, Liu Haipeng, Liu Juntao, Zhou Xiya, et al, 2019, Preliminary Study on the Efficient Electrohysterogram Segments for Recognizing Uterine Contractions with Convolutional Neural Networks, BioMed Research International, 2019(), 1, 10.1155/2019/3168541
- 4.Wang Hui, Wen Zichao, Wu Wenjie, Sun Zhexian, Kisrieva-Ware Zulfia, et al, 2023, Noninvasive electromyometrial imaging of human uterine maturation during term labor, Nature Communications, 14(1), 10.1038/s41467-023-36440-0